Costodiaphragmatic recess
| Costodiaphragmatic recess | |
|---|---|
 Chest X-ray of a 30-year-old healthy man, with the costodiaphragmatic recess label in red ellipse | |
 | |
| Details | |
| Identifiers | |
| Latin | Recessus costodiaphragmaticus |
| TA | A07.1.02.013 |
| FMA | 11355 |
The costodiaphragmatic recess, also called the costophrenic recess or phrenicocostal sinus,[1] is a potential space in the pleural cavity, at the posterior-most tips of the cavity, located at the junction of the costal pleura and diaphragmatic pleura (in the costophrenic angle). It measures approximately 5 cm vertically and extends from the eighth to the tenth rib along the mid-axillary line.
Function
The lungs expand into this recess during forced inspiration; however, the recess never fills completely. During expiration, it contains no lung tissue, only pleural fluid.
Clinical significance
Pleural effusions collect in the costodiaphragmatic recess when in standing position.[2]
A thoracocentesis (pleural tap) is often performed here while a patient is in full expiration because of less risk of puncturing the lungs and thereby causing pneumothorax.[2]
Imaging

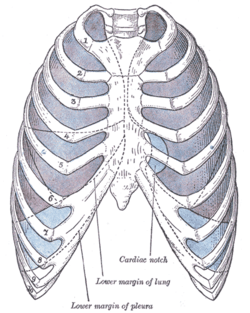
In anatomy, the costophrenic angles are the places where the diaphragm (-phrenic) meets the ribs (costo-).
Each costophrenic angle can normally be seen as on chest x-ray as a sharply-pointed, downward indentation (dark) between each hemi-diaphragm (white) and the adjacent chest wall (white). A small portion of each lung normally reaches into the costophrenic angle. The normal angle usually measures thirty degrees.
Pleural effusion
With pleural effusion, fluid often builds up in the costophrenic angle (due to gravity). This can push the lung upwards, resulting in "blunting" of the costophrenic angle. The posterior angle is the deepest. Obtuse angulation is sign of disease.
Chest x-ray is the first test done to confirm the presence of pleural fluid. The lateral upright chest x-ray should be examined when a pleural effusion is suspected. In an upright x-ray, 75 mL of fluid blunts the posterior costophrenic angle. Blunting of the lateral costophrenic angle usually requires about 175 mL but may take as much as 500 mL. Larger pleural effusions opacify portions of the hemithorax and may cause mediastinal shift; effusions > 4 L may cause complete opacification of the hemithorax and mediastinal shift to the contralateral side.
See also
References
This article incorporates text in the public domain from the 20th edition of Gray's Anatomy (1918)
- ↑ drugs.com > phrenicocostal-sinus Retrieved May 2011
- 1 2 drugs.com > costodiaphragmatic-recess Retrieved May 2011
External links
- 33947706 at GPnotebook
- Anatomy diagram: 02101.002-1 at Roche Lexicon - illustrated navigator, Elsevier
- Diagram (Question #4, item E)