Cocaine intoxication
| Cocaine intoxication | |
|---|---|
 | |
| Cocaine | |
| Classification and external resources | |
| Specialty | psychiatry |
| ICD-10 | F14.0 |
| ICD-9-CM | 305.6 |
| MedlinePlus | 000946 |
| eMedicine | article/813959 |
| MeSH | D019970 |
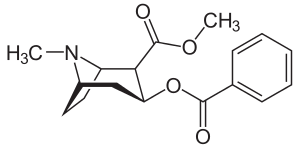
Cocaine intoxication refers to the immediate and deleterious effects of cocaine on the body. Although cocaine intoxication and cocaine dependence can be present in the same individual, these syndromes present with different symptoms.
Signs and symptoms
Cocaine increases alertness, feelings of well-being, euphoria, energy, competence, sociability, and sexuality. Common side effects include anxiety, increased temperature, paranoia, restlessness, and teeth grinding. With prolonged use, the drug can cause insomnia, anorexia, tachycardia, hallucinations, and paranoid delusions.[1] Possible lethal side effects include rapid heartbeat, abnormal heart rhythms, tremors, convulsions, markedly increased core temperature, renal failure, heart attack, stroke and heart failure.[2]
Depression with suicidal ideation may develop in heavy users.[3] Finally, a loss of vesicular monoamine transporters, neurofilament proteins, and other morphological changes appear to indicate a long-term damage to dopamine neurons.[4] Chronic intranasal usage can degrade the cartilage separating the nostrils (the septum nasi), which can eventually lead to its complete disappearance.[5]
Studies have shown that cocaine usage during pregnancy triggers premature labor[6] and may lead to abruptio placentae.[7]
Overdose
Cocaine can be snorted, swallowed, injected, or smoked. Most deaths due to cocaine are accidental but may also be the result of body packing or stuffing with rupture in the gastrointestinal tract. Use of cocaine causes tachyarrhythmias and a marked elevation of blood pressure (hypertension), which can be life-threatening. This can lead to death from acute myocardial infarction, respiratory failure, stroke, cerebral hemorrhage, or heart failure. Cocaine overdose may result in hyperthermia as stimulation and increased muscular activity cause greater heat production. Heat loss is also inhibited by the cocaine-induced vasoconstriction. Cocaine and/or associated hyperthermia may cause muscle cell destruction (rhabdomyolysis) and myoglobinuria resulting in renal failure. Individuals with cocaine overdose should be transported immediately to the nearest emergency department, preferably by ambulance in case cardiac arrest occurs en route. According to the National Institute on Drug Abuse, approximately 5000 deaths occur annually in the US due to cocaine overdose.[8]
Withdrawal
Physical withdrawal is not dangerous; however, physiological changes caused by cocaine withdrawal include vivid and unpleasant dreams, insomnia or hypersomnia, anger, increased appetite and psychomotor retardation or agitation. Cocaine and its metabolites are completely eliminated from the body by 3 days.[9]
Pathophysiology
Cocaine pharmacodynamics involve multiple complex mechanisms, although its half-life is short (~ 1 hour).[9] This drug binds and blocks monoamine (dopamine, epinephrine, norepinephrine, and serotonin) re-uptake transporters with equal affinity. Monoamines accumulate in the synaptic cleft resulting in enhanced and prolonged sympathetic effects. Cocaine's acute effect in the central nervous system is to raise the amount of dopamine and serotonin in the nucleus accumbens (the pleasure center in the brain). When this effect ceases due to metabolism of cocaine, depletion of associated neurotransmitters, and receptor down-regulation (tachyphylaxis), the cocaine user may experience dysphoria, or a "crash" after the initial high. The principal actions of cocaine on the cardiovascular system are from alpha- and beta-1-adrenoceptor stimulation resulting in increased heart rate, systemic arterial pressure, and myocardial contractility, which are major determinants of myocardial oxygen demand. Cocaine and its metabolites may cause arterial vasoconstriction hours after use. Epicardial coronary arteries are especially vulnerable to these effects, leading to decreased myocardial oxygen supply. Cocaine-induced platelet activation and thrombus formation is another deleterious effect, caused by alpha-adrenergic- and adenosine diphosphate-mediated increase in platelet aggregation.[10] Plasminogen activator inhibitor is also increased following cocaine use, thereby promoting thrombosis. Similar to local anesthetics such as lidocaine, cocaine blocks sodium channels and interferes with action potential propagation.[11] This Vaughn-Williams class IC effect increases the risk of conduction disturbance and tachyarrhythmias. Adding to its complex toxicity, cocaine targets muscarinic acetylcholine, N-methyl-D-aspartate (NMDA), sigma, and kappa-opioid receptors.[12][13][14][15]
Management
Emergency treatment of cocaine-associated hyperthermia consists of administering a benzodiazepine sedation agent, such as diazepam (Valium) or lorazepam (Ativan) to enhance muscle relaxation and decrease sympathetic outflow from the central nervous system. Physical cooling is best accomplished with tepid water misting and cooling with a fan (convection and evaporation), which can be carried out easily in the field or hospital.[16][17] There is no specific pharmacological antidote for cocaine overdose. The chest pain, high blood pressure, and increased heart rate caused by cocaine may be also treated with a benzodiazepine.[18] Multiple and escalating dose of benzodiazepines may be necessary to achieve effect, which increases risk of over-sedation and respiratory depression. A comprehensive systematic review of all pharmacological treatments of cocaine cardiovascular toxicity revealed benzodiazepines may not always reliably lower heart rate and blood pressure.[19]
Nitric-oxide mediated vasodilators, such as nitroglycerin and nitroprusside, are effective at lowering blood pressure and reversing coronary arterial vasoconstriction, but not heart rate.[19] Nitroglycerin is useful for cocaine-induced chest pain, but the possibility of reflex tachycardia must be considered.[20] Alpha-blockers such as phentolamine have been recommended[18] and may be used to treat cocaine-induced hypertension and coronary arterial vasoconstriction, but these agents do not reduce heart rate.[19][21] Furthermore, phentolamine is rarely used, not readily available in many emergency departments, and many present-day clinicians are unfamiliar with its use and titratability. Calcium channel blockers may also be used to treat hypertension and coronary arterial vasoconstriction,[22] but fail to lower tachycardia based on all cocaine-related studies.[19] Non-dihydropyridine calcium channels blockers such as diltiazem and verapamil are preferable, as dihydropyridine agents such as nifedipine have much higher risk of reflex tachycardia.
Agitated patients are best treated with benzodiazepines, but antipsychotics such as haloperidol and olanzapine may also be useful.[19] The alpha-2 agonist dexmedetomidine may also be useful for treatment of agitation, but effects on heart rate and blood pressure are variable based on several studies and case reports.[19] Lidocaine and intravenous lipid emulsion have been successfully used for serious ventricular tachyarrhythmias in several case reports.
The use of beta-blockers for cocaine cardiovascular toxicity has been subject to a relative contraindication by many clinicians for several years despite extremely limited evidence. The phenomenon of “unopposed alpha-stimulation,” in which blood pressure increases or coronary artery vasoconstriction worsens after blockade of beta-2 vasodilation in cocaine-abusing patients, is controversial.[23][24] This rarely-encountered and unpredictable adverse effect has resulted in some clinicians advocating for an absolute contraindication of the use of all beta-blockers, including specific, non-specific, and mixed.[25] Many clinicians have disregarded this dogma and administer beta-blockers for cocaine-related chest pain and acute coronary syndrome, especially when there is demand ischemia from uncontrolled tachycardia.[26][27][28][29][30] Of the 1,744 total patients identified in the aforementioned systematic review,[19] only 7 adverse events were from putative cases of “unopposed alpha-stimulation” due to propranolol (n=3), esmolol (n=3), and metoprolol (n=1).[31][32][33][34][35] Some detractors of beta-blockers for cocaine-induced chest pain have cited minimal acute mortality and the short half-life of the drug, making it unnecessary to aggressively treat any associated tachycardia and hypertension.[25][36] However, the long-term effect of cocaine use and development of heart failure, with early mortality, high morbidity, and tremendous demand on hospital utilization should be taken under consideration.[37][38][39]
The mixed beta/alpha blocker labetalol has been shown to be safe and effective for treating concomitant cocaine-induced hypertension and tachycardia, without any “unopposed alpha-stimulation” adverse events recorded.[19][40][41] The use of labetalol is approved by a recent AHA/ACC guideline for cocaine and methamphetamine patients with unstable angina/non-STEMI.[42]
References
- ↑ Glauser, Jonathan; Queen, John R. (2007-02-01). "An overview of non-cardiac cocaine toxicity". The Journal of Emergency Medicine. 32 (2): 181–186. doi:10.1016/j.jemermed.2006.05.044. ISSN 0736-4679. PMID 17307630.
- ↑ Zimmerman, Janice L. (2012-10-01). "Cocaine intoxication". Critical Care Clinics. 28 (4): 517–526. doi:10.1016/j.ccc.2012.07.003. ISSN 1557-8232. PMID 22998988.
- ↑ Narvaez, Joana C. M.; Jansen, Karen; Pinheiro, Ricardo T.; Kapczinski, Flávio; Silva, Ricardo A.; Pechansky, Flávio; Magalhães, Pedro V. (2014-08-01). "Psychiatric and substance-use comorbidities associated with lifetime crack cocaine use in young adults in the general population". Comprehensive Psychiatry. 55 (6): 1369–1376. doi:10.1016/j.comppsych.2014.04.021. ISSN 1532-8384. PMID 24933652.
- ↑ Little, Karley Y.; Ramssen, Eric; Welchko, Ryan; Volberg, Vitaly; Roland, Courtney J.; Cassin, Bader (2009-08-15). "Decreased brain dopamine cell numbers in human cocaine users". Psychiatry Research. 168 (3): 173–180. doi:10.1016/j.psychres.2008.10.034. ISSN 0165-1781. PMID 19233481.
- ↑ Trimarchi, M.; Bussi, M.; Sinico, R. A.; Meroni, Pierluigi; Specks, U. (2013-02-01). "Cocaine-induced midline destructive lesions - an autoimmune disease?". Autoimmunity Reviews. 12 (4): 496–500. doi:10.1016/j.autrev.2012.08.009. ISSN 1873-0183. PMID 22940554.
- ↑ Cain, Mary A.; Bornick, Patricia; Whiteman, Valerie (2013-03-01). "The maternal, fetal, and neonatal effects of cocaine exposure in pregnancy". Clinical Obstetrics and Gynecology. 56 (1): 124–132. doi:10.1097/GRF.0b013e31827ae167. ISSN 1532-5520. PMID 23314714.
- ↑ Flowers, D.; Clark, J. F.; Westney, L. S. (1991-03-01). "Cocaine intoxication associated with abruptio placentae.". Journal of the National Medical Association. 83 (3): 230–232. ISSN 0027-9684. PMC 2627035
 . PMID 2038082.
. PMID 2038082. - ↑ "Unintentional Drug Poisoning in the United States" (PDF). Centers for Disease Control and Prevention. 2010-07-01. Retrieved 2012-06-11.
- 1 2 Jufer, R. A.; Wstadik, A.; Walsh, S. L.; Levine, B. S.; Cone, E. J. (2000-10-01). "Elimination of cocaine and metabolites in plasma, saliva, and urine following repeated oral administration to human volunteers". Journal of Analytical Toxicology. 24 (7): 467–477. doi:10.1093/jat/24.7.467. ISSN 0146-4760. PMID 11043648.
- ↑ Heesch, C. M.; Wilhelm, C. R.; Ristich, J.; Adnane, J.; Bontempo, F. A.; Wagner, W. R. (2000-06-01). "Cocaine activates platelets and increases the formation of circulating platelet containing microaggregates in humans". Heart (British Cardiac Society). 83 (6): 688–695. doi:10.1136/heart.83.6.688. ISSN 1468-201X. PMC 1760877
 . PMID 10814631.
. PMID 10814631. - ↑ Hariman, Robert J.; Liu, Dong; Loeb, Henry S.; McKieman, Thomas L.; Scanlon, Patrick J.; Bauman, Jerry L. (1996-02-01). "Competitive binding between cocaine and lidocaine". Journal of the American College of Cardiology. 27 (2): 80. doi:10.1016/S0735-1097(96)80520-1.
- ↑ Williams, Mark J.; Adinoff, Bryon (2008-07-01). "The role of acetylcholine in cocaine addiction". Neuropsychopharmacology: Official Publication of the American College of Neuropsychopharmacology. 33 (8): 1779–1797. doi:10.1038/sj.npp.1301585. ISSN 0893-133X. PMC 2667818
 . PMID 17928814.
. PMID 17928814. - ↑ Haile, Colin N.; Mahoney, James J.; Newton, Thomas F.; De La Garza, Richard (2012-05-01). "Pharmacotherapeutics directed at deficiencies associated with cocaine dependence: focus on dopamine, norepinephrine and glutamate". Pharmacology & Therapeutics. 134 (2): 260–277. doi:10.1016/j.pharmthera.2012.01.010. ISSN 1879-016X. PMC 3341931
 . PMID 22327234.
. PMID 22327234. - ↑ Narayanan, Sanju; Mesangeau, Christophe; Poupaert, Jacques H.; McCurdy, Christopher R. (2011-01-01). "Sigma receptors and cocaine abuse". Current Topics in Medicinal Chemistry. 11 (9): 1128–1150. doi:10.2174/156802611795371323. ISSN 1873-4294. PMID 21050176.
- ↑ Kivell, Bronwyn M.; Ewald, Amy W. M.; Prisinzano, Thomas E. (2014-01-01). "Salvinorin A analogs and other κ-opioid receptor compounds as treatments for cocaine abuse". Advances in Pharmacology. 69: 481–511. doi:10.1016/B978-0-12-420118-7.00012-3. ISSN 1557-8925. PMC 4128345
 . PMID 24484985.
. PMID 24484985. - ↑ Smith, Caroline J.; Johnson, John M. (2016-04-01). "Responses to hyperthermia. Optimizing heat dissipation by convection and evaporation: Neural control of skin blood flow and sweating in humans". Autonomic Neuroscience: Basic & Clinical. 196: 25–36. doi:10.1016/j.autneu.2016.01.002. ISSN 1872-7484. PMID 26830064.
- ↑ Richards, John R.; Colby, Daniel K. (2016-01-01). "Stimulant-induced hyperthermia and ice-water submersion: Practical considerations". Clinical Toxicology (Philadelphia, Pa.). 54 (1): 69–70. doi:10.3109/15563650.2015.1104536. ISSN 1556-9519. PMID 26515112.
- 1 2 McCord, J; Jneid, H; Hollander, JE; de Lemos, JA; Cercek, B; Hsue, P; Gibler, WB; Ohman, EM; Drew, B; Philippides, G; Newby, LK; American Heart Association Acute Cardiac Care Committee of the Council on Clinical, Cardiology (Apr 8, 2008). "Management of cocaine-associated chest pain and myocardial infarction: a scientific statement from the American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology.". Circulation. 117 (14): 1897–907. doi:10.1161/CIRCULATIONAHA.107.188950. PMID 18347214.
- 1 2 3 4 5 6 7 8 Richards, John R.; Garber, Dariush; Laurin, Erik G.; Albertson, Timothy E.; Derlet, Robert W.; Amsterdam, Ezra A.; Olson, Kent R.; Ramoska, Edward A.; Lange, Richard A. (2016-06-01). "Treatment of cocaine cardiovascular toxicity: a systematic review". Clinical Toxicology (Philadelphia, Pa.). 54 (5): 345–364. doi:10.3109/15563650.2016.1142090. ISSN 1556-9519. PMID 26919414.
- ↑ Ma, Sheng-xing; Schmid, Phillip G.; Long, John P. (1994-01-01). "Noradrenergic mechanisms and the cardiovascular actions of nitroglycerin". Life Sciences. 55 (21): 1595–1603. doi:10.1016/0024-3205(94)00325-4.
- ↑ Lange, Richard A.; Cigarroa, Ricardo G.; Yancy, Clyde W. Jr.; Willard, John E.; Popma, Jeffrey J.; Sills, Michael N.; McBride, Wade; Kim, Anatole S.; Hillis, L. David (1989-12-07). "Cocaine-Induced Coronary-Artery Vasoconstriction". New England Journal of Medicine. 321 (23): 1557–1562. doi:10.1056/NEJM198912073212301. ISSN 0028-4793. PMID 2573838.
- ↑ Negus, Brian H.; Willard, John E.; Hillis, L.David; Glamann, D.Brent; Landau, Charles; Snyder, Richard W.; Lange, Richard A. (1994-03-01). "Alleviation of cocaine-induced coronary vasoconstriction with intravenous verapamil". The American Journal of Cardiology. 73 (7): 510–513. doi:10.1016/0002-9149(94)90684-x. ISSN 0002-9149.
- ↑ Schurr, James W.; Gitman, Brenda; Belchikov, Yuly (2014-12-01). "Controversial therapeutics: the β-adrenergic antagonist and cocaine-associated cardiovascular complications dilemma". Pharmacotherapy. 34 (12): 1269–1281. doi:10.1002/phar.1486. ISSN 1875-9114. PMID 25224512.
- ↑ Freeman, Kalev; Feldman, James A. (2008-02-01). "Cocaine, myocardial infarction, and beta-blockers: time to rethink the equation?". Annals of Emergency Medicine. 51 (2): 130–134. doi:10.1016/j.annemergmed.2007.08.020. ISSN 1097-6760. PMID 17933425.
- 1 2 Gupta, Amit K.; Greller, Howard A.; Hoffman, Robert Steven (2010-11-08). "Beta-blockers and cocaine: still a bad idea". Archives of Internal Medicine. 170 (20): 1859–1860; author reply 1860. doi:10.1001/archinternmed.2010.398. ISSN 1538-3679. PMID 21059982.
- ↑ Dattilo, Philip B.; Hailpern, Susan M.; Fearon, Kerrie; Sohal, Davendra; Nordin, Charles (2008-02-01). "Beta-blockers are associated with reduced risk of myocardial infarction after cocaine use". Annals of Emergency Medicine. 51 (2): 117–125. doi:10.1016/j.annemergmed.2007.04.015. ISSN 1097-6760. PMID 17583376.
- ↑ Rangel, Carlos; Shu, Richard G.; Lazar, Lawrence D.; Vittinghoff, Eric; Hsue, Priscilla Y.; Marcus, Gregory M. (2010-05-24). "Beta-blockers for chest pain associated with recent cocaine use". Archives of Internal Medicine. 170 (10): 874–879. doi:10.1001/archinternmed.2010.115. ISSN 1538-3679. PMID 20498415.
- ↑ Ibrahim, Morhaf; Maselli, Diego Jose; Hasan, Reham; Hamilton, Andrew (2013-03-01). "Safety of β-blockers in the acute management of cocaine-associated chest pain". The American Journal of Emergency Medicine. 31 (3): 613–616. doi:10.1016/j.ajem.2012.09.027. ISSN 1532-8171. PMID 23122421.
- ↑ Fanari, Zaher; Kennedy, Kevin K.; Lim, Michael J.; Laddu, Abhay A.; Stolker, Joshua M. (2014-06-01). "Comparison of in-hospital outcomes for beta-blocker use versus non-beta blocker use in patients presenting with cocaine-associated chest pain". The American Journal of Cardiology. 113 (11): 1802–1806. doi:10.1016/j.amjcard.2014.03.010. ISSN 1879-1913. PMID 24742472.
- ↑ Gupta, Navdeep; Washam, Jeffrey B.; Mountantonakis, Stavros E.; Li, Shuang; Roe, Matthew T.; de Lemos, James A.; Arora, Rohit (2014-03-01). "Characteristics, management, and outcomes of cocaine-positive patients with acute coronary syndrome (from the National Cardiovascular Data Registry)". The American Journal of Cardiology. 113 (5): 749–756. doi:10.1016/j.amjcard.2013.11.023. ISSN 1879-1913. PMID 24388623.
- ↑ Ramoska, Edward; Sacchetti, Alfred D (1985-11-01). "Propranolol-induced hypertension in treatment of cocaine intoxication". Annals of Emergency Medicine. 14 (11): 1112–1113. doi:10.1016/s0196-0644(85)80934-3. ISSN 0196-0644.
- ↑ Fareed, Fareed N.; Chan, Gar; Hoffman, Robert S. (2007-12-01). "Death temporally related to the use of a Beta adrenergic receptor antagonist in cocaine associated myocardial infarction". Journal of Medical Toxicology: Official Journal of the American College of Medical Toxicology. 3 (4): 169–172. doi:10.1007/bf03160934. ISSN 1556-9039. PMC 3550023
 . PMID 18072171.
. PMID 18072171. - ↑ Sand, I.Charles; Brody, Steven L.; Wrenn, Keith D.; Slovis, Corey M. (1991-03-01). "Experience with esmolol for the treatment of cocaine-associated cardiovascular complications". The American Journal of Emergency Medicine. 9 (2): 161–163. doi:10.1016/0735-6757(91)90182-j. ISSN 0735-6757.
- ↑ Lange, Richard A.; Cigarroa, Ricardo G.; Flores, Eduardo D.; McBride, Wade; Kim, Anatole S.; Wells, Peter J.; Bedotto, John B.; Danziger, Robert S.; Hillis, L. David (1990-06-15). "Potentiation of Cocaine-Induced Coronary Vasoconstriction by Beta-Adrenergic Blockade". Annals of Internal Medicine. 112 (12): 897–903. doi:10.7326/0003-4819-112-12-897. ISSN 0003-4819.
- ↑ Izquierdo Gómez, María Manuela; Domínguez-Rodríguez, Alberto; Gálvez Rodríguez, Manuel; Marrero Rodríguez, Francisco (2009-04-01). "Reflections on beta-adrenergic receptor blockers and cocaine use. A case in point". Revista Española De Cardiología. 62 (4): 455–456. doi:10.1016/s1885-5857(09)71677-9. ISSN 1579-2242. PMID 19401135.
- ↑ Hollander, Judd (December 28, 2011). "Update on Cocaine Myocardial Ischemia".
- ↑ Casartelli, Alessandro; Dacome, Lisa; Tessari, Michela; Pascali, Jennifer; Bortolotti, Federica; Trevisan, Maria Teresa; Bosco, Oliviero; Cristofori, Patrizia; Tagliaro, Franco (2014-01-01). "Cocaine-associated increase of atrial natriuretic peptides: an early predictor of cardiac complications in cocaine users?". Heart Asia. 6 (1): 100–107. doi:10.1136/heartasia-2013-010482. ISSN 1759-1104. PMC 4832714
 . PMID 27326180.
. PMID 27326180. - ↑ Liaudet, Lucas; Calderari, Belinda; Pacher, Pal (2014-11-01). "Pathophysiological mechanisms of catecholamine and cocaine-mediated cardiotoxicity". Heart Failure Reviews. 19 (6): 815–824. doi:10.1007/s10741-014-9418-y. ISSN 1573-7322. PMID 24398587.
- ↑ Walsh, David W.; McVey, Molly C.; Gass, Abigal; Zhang, Jingwen; Mauldin, Patrick D.; Rockey, Don C. (2016-06-24). "Identification of high resource utilizing patients on internal medicine hospital services". Journal of Investigative Medicine: The Official Publication of the American Federation for Clinical Research: jim–2016–000118. doi:10.1136/jim-2016-000118. ISSN 1708-8267. PMID 27342424.
- ↑ Boehrer, James D.; Moliterno, David J.; Willard, John E.; Hillis, L.David; Lange, Richard A. (1993-06-01). "Influence of labetalol on cocaine-induced coronary vasoconstriction in humans". The American Journal of Medicine. 94 (6): 608–610. doi:10.1016/0002-9343(93)90212-8. ISSN 0002-9343.
- ↑ Richards, John R.; Lange, Richard A. (2016-02-01). "Labetalol and cardiovascular consequences of cocaine use". Trends in Cardiovascular Medicine. 26 (2): 202–203. doi:10.1016/j.tcm.2015.05.002. ISSN 1873-2615. PMID 26116092.
- ↑ Anderson, Jeffrey L.; Adams, Cynthia D.; Antman, Elliott M.; Bridges, Charles R.; Califf, Robert M.; Casey, Donald E.; Chavey, William E.; Fesmire, Francis M.; Hochman, Judith S. (2013-06-11). "2012 ACCF/AHA focused update incorporated into the ACCF/AHA 2007 guidelines for the management of patients with unstable angina/non-ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines". Journal of the American College of Cardiology. 61 (23): e179–347. doi:10.1016/j.jacc.2013.01.014. ISSN 1558-3597. PMID 23639841.
- ↑ How long does cocaine stay in your system - Dr. GoodEarth Journal