Cauda equina syndrome
| Cauda equina syndrome | |
|---|---|
|
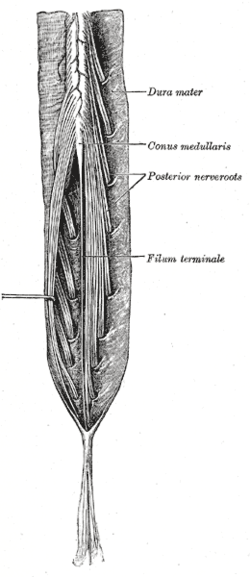
Cauda equina and filum terminale seen from behind. | |
| Classification and external resources | |
| Specialty | Neurosurgery, orthopedics |
| ICD-10 | G83.4 |
| ICD-9-CM | 344.6 |
| DiseasesDB | 31115 |
| eMedicine | emerg/85 orthoped/39 |
| MeSH | C10.668.829.800.750.700 |
Cauda equina syndrome (CES) is a serious neurologic condition in which damage to the cauda equina causes loss of function of the lumbar plexus (nerve roots) of the spinal canal below the termination (conus medullaris) of the spinal cord. CES is a lower motor neuron lesion.
Signs and symptoms
- Severe back pain
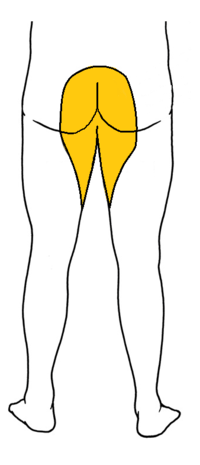
- Saddle anesthesia (see diagram), i.e., anesthesia or paraesthesia involving S3 to S5 dermatomes,[1]:26 including the perineum, external genitalia and anus; or more descriptively, numbness or "pins-and-needles" sensations of the groin and inner thighs which would contact a saddle when riding a horse.
- Bladder and bowel dysfunction,[2]:216 caused by decreased tone of the urinary and anal sphincters. Detrusor weaknesses causing urinary retention and post-void residual incontinence as assessed by bladder scanning the patient after the patient has urinated.
- Sciatica-type pain on one side or both sides, although pain may be wholly absent
- Weakness of the muscles of the lower legs (often paraplegia)
- Achilles (ankle) reflex absent on both sides.[2]:216
- Sexual dysfunction
- Absent anal reflex and bulbocavernosus reflex
- Gait disturbance
Severe back pain, saddle anesthesia, incontinence and sexual dysfunction are considered "red flags", i.e. features which require urgent investigation.[3]
Causes
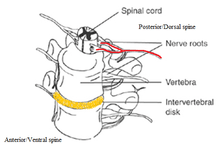
After the conus medullaris, the canal contains a mass of nerves (the cauda equina or "horse-tail") that branches off the lower end of the spinal cord and contains the nerve roots from L1-5 and S1-5. The nerve roots from L4-S4 join in the sacral plexus which affects the sciatic nerve, which travels caudally (toward the feet). Compression, trauma or other damage to this region of the spinal canal can result in cauda equina syndrome.
The symptoms may also appear as a temporary side-effect of a sacral extra-dural injection:[4]
Tumors and lesions
Any lesion which compresses or disturbs the function of the cauda equina may disable the nerves although the most common is a central disc prolapse. Metastatic disease may also be a cause.[5]
Trauma
Direct trauma can also cause cauda equina syndrome. Most common causes include iatrogenic lumbar punctures, burst fractures resulting in posterior migration of fragments of the vertebral body, severe disc herniations, spinal anaesthesia involving trauma from catheters and high local anaesthetic concentrations around the cauda equina, penetrating trauma such as knife wounds or ballistic trauma.[6]
Spinal stenosis
CES can be caused by lumbar spinal stenosis, which is when the diameter of the spinal canal narrows. This could be the result of a degenerative process of the spine (such as osteoarthritis) or a developmental defect which is present at birth. In the most severe cases of spondylolisthesis cauda equina syndrome can result.[6]
Inflammatory conditions
Chronic spinal inflammatory conditions such as Paget disease, neurosarcoidosis, chronic inflammatory demyelinating polyneuropathy, ankylosing spondylitis and chronic tuberculosis can cause it. This is due to the spinal canal narrowing that these kind of syndromes can produce.[6]
Risk factors
No set risk factors have been clearly defined for CES at this point in time.[7] Individuals most at risk for disc herniation are the most likely to develop CES. Race has little influence with the notable exception that African Americans appear slightly less likely to develop CES than other groups; similarly, men are slightly more likely to develop CES than women.[7][8][9] Middle age also appears to be a notable risk factor, as those populations are more likely to develop a herniated disc; heavy lifting can also be inferred as a risk factor for CES.[7][9]
Diagnosis
Examination for pain sensation, by pinprick, shows leg (lumbar nerves) analgesia with perineal (sacral nerves) escape. The maintenance of perineal sensation with absence of pain sensation over the lumbar nerve roots is typical for an extra-medullary and intra-thecal (outside the cord and within the dural sheath) process. Inability to walk, with this unusual sensory examination completes a triad of signs and usually represents spinal tuberculosis. The triad is paraplegia with lumbar loss of pain sensation and presence of perineal altered sensation.
Diagnosis is usually confirmed by an MRI scan or CT scan, depending on availability. If cauda equina syndrome exists, it is unclear whether early surgery confers extra benefit. Although early surgery in acute onset of severe cases has been reported to be important.[10]
Prevention
Early diagnosis can allow for preventive treatment. Signs that allow early diagnosis include changes in bowel and bladder function and loss of feeling in groin.[11]
Management
The management of true cauda equina syndrome frequently involves surgical decompression. When cauda equina syndrome is caused by a herniated disk early surgical decompression is recommended.[12]
Cauda equina syndrome of sudden onset is regarded as a medical/surgical emergency.[13] Surgical decompression by means of laminectomy or other approaches may be undertaken within 6,[14] 24[15][16] or 48 hours of symptoms developing if a compressive lesion, e.g., ruptured disc, epidural abscess, tumour or haematoma is demonstrated. Early treatment may significantly improve the chance that long-term neurological damage will be avoided.[12][16]
Surgery may be required to remove blood, bone fragments, a tumor or tumors, a herniated disc or an abnormal bone growth. If the tumor cannot be removed surgically and it is malignant then radiotherapy may be used as an alternative to relieve pressure, with spinal neoplasms chemotherapy can also be used. If the syndrome is due to an inflammatory condition e.g., ankylosing spondylitis, anti-inflammatory, including steroids can be used as an effective treatment. If a bacterial infection is the cause then an appropriate course of antibiotics can be used to treat it.[17]
Cauda equina syndrome can occur during pregnancy due to lumbar disc herniation; age of mother increases the risk. Surgery can still be performed and the pregnancy does not adversely affect treatment. Treatment for those with cauda equina can and should be carried out at any time during pregnancy.[18]
Lifestyle issues may need to be addressed post - treatment. Issues could include the patients need for physiotherapy and occupational therapy due to lower limb dysfunction. Obesity might also need to be tackled.[17]
Rehabilitation
Physical therapy can be somewhat useful for patient’s recovery from surgery (Kennedy, Soffee, McGrath, Stephens, Walsh, & McManus, 1999). The main focus of rehabilitation is centered on controlling the bladder and bowel functions and decreasing muscle weakness in the lower extremities.
Bowel and bladder control
Rehabilitation of CES depends on the severity of the injury. If permanent damage occurs, then impairment in bladder and bowel control may result (Hodges, 2004 ). Once surgery is performed, resting is required until the bladder and bowel dysfunction can be assessed (Hodges, 2004 ). Urinary catheterization may help with bladder control (Hodges, 2004). Gravity and exercise can help control bowel movement (Hodges, 2004). Pelvic floor exercises assist in controlling bowel movements (Pelvic Floor Exercises, 2010). These exercises can be done standing, lying, or on all fours with the knees slightly separated (Fig. 2). Full recovery of bowel and bladder control can take as long as two years (Hodges, 2004).
Physical Therapy
Physical therapist can assist in sitting stability, and transferring by working on strength training. Therapists will work on balance, gait, and transfers since muscle weakness or paralysis may occur in the lower extremities (Dawodu, 2013). Additionally, electrical stimulation is also helpful to enhance muscle tone (Dawodu, 2013).
Prognosis
The prognosis for complete recovery is dependent upon many factors. The most important of these is the severity and duration of compression upon the damaged nerve(s). Generally, the longer the time before intervention to remove the compression causing nerve damage, the greater the damage caused to the nerve(s).
Damage can be so severe that nerve regrowth is impossible, and the nerve damage will be permanent. In cases where the nerve has been damaged but is still capable of regrowth, recovery time is widely variable. Surgical intervention with decompression of the cauda equina can assist recovery. Delayed or severe nerve damage can mean up to several years' recovery time because nerve growth is exceptionally slow.
Review of the literature indicates that around 50-70% of patients have urinary retention (CES-R) on presentation with 30-50% having an incomplete syndrome (CES-I). The latter group, especially if the history is less than a few days, usually requires emergency MRI to confirm the diagnosis followed by prompt decompression. CES-I with its more favourable prognosis may become CES-R at a later stage.[19]
Epidemiology
Various etiologies of CES include fractures, abscesses, hematomas, and any compression of the relevant nerve roots.[20] Injuries to the thoracolumbar spine will not necessarily result in a clinical diagnosis of CES, but in all such cases it is necessary to consider. Few epidemiological studies of CES have been done in the United States, owing to difficulties such as amassing sufficient cases as well as defining the affected population, therefore this is an area deserving of additional scrutiny.[7]
Traumatic spinal cord injuries occur in approximately 40 people per million annually in the United States, resulting from traumas due to motor vehicle accidents, sporting injuries, falls, and other factors.[8] An estimated 10 to 25% of vertebral fractures will result in injury to the spinal cord.[8] Thorough physical examinations are required, as 5 to 15% of trauma patients have fractures that initially go undiagnosed.[21]
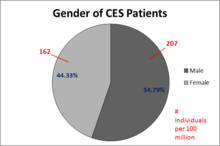
The most frequent injuries of the thoracolumbar region are to the conus medullaris and the cauda equina, particularly between T12 and L2.[8] Of these two syndromes, CES is the more common.[8] CES mainly affects middle-aged individuals, particularly those in their forties and fifties, and presents more often in men.[8][9][22] It is not a typical diagnosis, developing in only 4 to 7 out of every 10,000 to 100,000 patients, and is more likely to occur proximally.[7][8][9] Disc herniation is reportedly the most common cause of CES, and it is thought that 1 to 2% of all surgical disc herniation cases result in CES.[7][8]
Cost
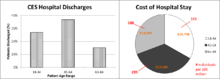
CES is often concurrent with congenital or degenerative diseases and represents a high cost of care to those admitted to the hospital for surgery.[8][22] Hospital stays generally last 4 to 5 days, and cost an average of $100,000 to $150,000,[22] unless the patient lives in a country where healthcare is free at the point of demand.
References
- ↑ Larner, A.J. (2006). A Dictionary of Neurological Signs (2nd ed.). [New York]: Springer Science+Business Media, Inc. ISBN 9780387262147.
- 1 2 Kraemer, Juergen; Christiane,; Solodkoff, Michael von (2009). Intervertebral disk diseases causes, diagnosis, treatment, and prophylaxis (3rd ed.). Stuttgart: Thieme. ISBN 9783131495617.
- ↑ Gardner, Alan; Gardner, Edward; Morley, Tim (31 December 2010). "Cauda equina syndrome: a review of the current clinical and medico-legal position". European Spine Journal. 20 (5): 690–697. doi:10.1007/s00586-010-1668-3.
- ↑ Gerald L Burke,MD. "Backache from Occiput to Coccyx". Retrieved 2014-07-23.
- ↑ Walid MS, Ajjan M, Johnston KW, Robinson JS (2008). "Cauda Equina Syndrome—Think of Cancer". The Permanente Journal. 12 (2): 48–51. ISSN 1552-5767. PMC 3042291
 . PMID 21364812.
. PMID 21364812. - 1 2 3 Eck, Jason C (11 May 2007). "Cauda Equina Syndrome Causes". Cauda Equina Syndrome. WebMD. Retrieved 25 April 2009.
- 1 2 3 4 5 6 Schoenfeld, A.J.; Bader, J.O. (2012). "Cauda equina syndrome: an analysis of incidence rates and risk factors among a closed North American military population". Clinical Neurology and Neurosurgery. 114: 947–950. doi:10.1016/j.clineuro.2012.02.012.
- 1 2 3 4 5 6 7 8 9 Radcliff, K.E.; Kepler, C.K.; Delasotta, L.A.; Rihn, J.A.; Harrop, J.S.; Hilibrand, A.S.; Albert, T.J.; Vaccaro, A.R. (2011). "Current management review of thoracolumbar cord syndromes". Spine. 11: 884–892. doi:10.1016/j.spinee.2011.07.022.
- 1 2 3 4 Small, S.A.; Perron, A.D.; Brady, W.J. (2005). "Orthopedic pitfalls: cauda equina syndrome". American Journal of Emergency Medicine. 23: 159–163. doi:10.1016/j.ajem.2004.03.006.
- ↑ Shapiro S (February 2000)
- ↑ Eck, Jason C (11 May 2007). "Prevention". Cauda Equina Syndrome. WebMD. Retrieved 25 April 2009.
- 1 2 Ahn UM, Ahn NU, Buchowski JM, Garrett ES, Sieber AN, Kostuik JP (June 2000). "Cauda equina syndrome secondary to lumbar disc herniation: a meta-analysis of surgical outcomes". Spine. 25 (12): 1515–22. doi:10.1097/00007632-200006150-00010. PMID 10851100.
- ↑ Shapiro S (February 2000). "Medical realities of cauda equina syndrome secondary to lumbar disc herniation". Spine. 25 (3): 348–51; discussion 352. doi:10.1097/00007632-200002010-00015. PMID 10703108.
- ↑ "Neurosurgery for Cauda Equina Syndrome". Medscape. Nov 11, 2013. Retrieved 18 March 2015.
- ↑ "Late Decompression Of Cauda Equina Syndrome: Is It Worthwhile? Report Of Two Cases.". The Internet Journal of Spine Surgery. 2009. Retrieved 18 March 2015.
- 1 2 "Delayed presentation of cauda equina syndrome secondary to lumbar disc herniation: functional outcomes and health-related quality of life". Canadian Association of Emergency Physicians. July 10, 2001. Retrieved 18 March 2015.
- 1 2 Tidy, Colin (16 Nov 2009). "Cauda Equina Syndrome". Egton Medical Information Systems. Retrieved 11 January 2010.
- ↑ Brown MD, Levi AD (February 2001). "Surgery for lumbar disc herniation during pregnancy". Spine. 26 (4): 440–3. doi:10.1097/00007632-200102150-00022. PMID 11224893.
- ↑ ADH Gardner, EMH Gardner, TR Morley (2011). Cauda equina syndrome: a review of the current clinical and medico-legal position European Spine Journal; Vol. 20 Number 5, May 2011
- ↑ Gitelman, A.; Hishmeh, S.; Morelli, B.N.; Joseph Jr., S.A.; Casden, A.; Kuflik, P.; Neuwirth, M.; Stephen, M. (2008). "Cauda equina syndrome: a comprehensive review". The American Journal of Orthopedics. 37 (11): 556–562.
- ↑ Harrop, J.S.; Hunt Jr., G.E.; Vaccaro, A.R. (2004). "Conus medullaris and cauda equina syndrome as a result of traumatic injuries: management principles". Neurosurgery Focus. 16: 19–23. doi:10.3171/foc.2004.16.6.4.
- 1 2 3 "National and regional estimates on hospital use for all patients from the HCUP nationwide inpatient sample (NIS)". United States Department of Health and Human Services Agency for Healthcare Research. 2012.
External links
- 06-093c. at Merck Manual of Diagnosis and Therapy Home Edition
- Cauda_equina_syndrome at the Duke University Health System's Orthopedics program
- http://www.caudaequinauk.com/welcome.php Cauda Equina Syndrome UK Charity's social network