Bronchopulmonary dysplasia
| Bronchopulmonary dysplasia | |
|---|---|
|
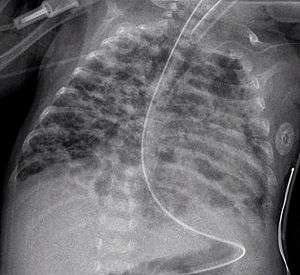
a radiograph of bronchopulmonary dysplasia | |
| Classification and external resources | |
| Specialty | pediatrics |
| ICD-10 | P27.1 |
| ICD-9-CM | 770.7 |
| DiseasesDB | 1713 |
| MedlinePlus | 001088 |
| eMedicine | ped/289 |
| Patient UK | Bronchopulmonary dysplasia |
| MeSH | D001997 |
Bronchopulmonary dysplasia (BPD; formerly chronic lung disease of infancy) is a chronic lung disorder of infants and children first described in 1967. It is more common in infants with low birth weight and those who receive prolonged mechanical ventilation to treat respiratory distress syndrome (RDS). It results in significant morbidity and mortality. The definition of BPD has continued to evolve since then primarily due to changes in the population, such as more survivors at earlier gestational ages, and improved neonatal management including surfactant, antenatal glucocorticoid therapy, and less aggressive mechanical ventilation.[1]
Currently the description of BPD includes the grading of its severity into mild, moderate and severe. This correlates with the infant's maturity, growth and overall severity of illness.[2] The new system offers a better description of underlying pulmonary disease and its severity.[3]
Diagnosis
Earlier criteria
The classic diagnosis of BPD may be assigned at 28 days of life if the following criteria are met:
- Positive pressure ventilation during the first 2 weeks of life for a minimum of 3 days.
- Clinical signs of abnormal respiratory function.
- Requirements for supplemental oxygen for longer than 28 days of age to maintain PaO2 above 50 mm Hg.
- Chest radiograph with diffuse abnormal findings characteristic of BPD.
Newer criteria
The newer National Institute of Health (US) criteria for BPD (for neonates treated with more than 21% oxygen for at least 28 days)[4] is as follows:,[5][6]
- Mild
- Breathing room air at 36 weeks post-menstrual age or discharge (whichever comes first) for babies born before 32 weeks, or
- breathing room air by 56 days postnatal age, or discharge (whichever comes first) for babies born after 32 weeks gestation.
- Moderate
- Need for <30% oxygen at 36 weeks postmenstrual age, or discharge (whichever comes first) for babies born before 32 weeks, or
- need for <30% oxygen to 56 days postnatal age, or discharge (whichever comes first) for babies born after 32 weeks gestation.
- Severe
- Need for >30% oxygen, with or without positive pressure ventilation or continuous positive pressure at 36 weeks postmenstrual age, or discharge (whichever comes first) for babies born before 32 weeks, or
- need for >30% oxygen with or without positive pressure ventilation or continuous positive pressure at 56 days postnatal age, or discharge (whichever comes first) for babies born after 32 weeks' gestation.
Cause and manifestations
Prolonged high oxygen delivery in premature infants causes necrotizing bronchiolitis and alveolar septal injury, with inflammation and scarring. This results in hypoxemia. Today, with the advent of surfactant therapy and high frequency ventilation and oxygen supplementation, infants with BPD experience much milder injury without necrotizing bronchiolitis or alveolar septal fibrosis. Instead, there are usually uniformly dilated acini with thin alveolar septa and little or no interstitial fibrosis. It develops most commonly in the first 4 weeks after birth.
Complications
Feeding problems are common in infants with BPD, often due to prolonged intubation. Such infants often display oral-tactile hypersensitivity (also known as oral aversion).[7] Physical findings:
- hypoxemia;
- hypercapnia;
- crackles, wheezing, & decreased breath sounds;
- increased bronchial secretions;
- hyperinflation;
- frequent lower respiratory infections;
- delayed growth & development;
- cor pulmonale;
- CXR shows with hyperinflation, low diaphragm, atelectasis, cystic changes.
Management
There is evidence to show that steroids given to babies less than 8 days old can prevent bronchopulmonary dysplasia. However, the risks of treatment may outweigh the benefits.[8] It is unclear if starting steroids more than 7 days after birth is harmful or beneficial. It is thus recommended that they only be used in those who cannot be taken off of a ventilator.[9]
Epidemiology
The rate of BPD varies among institutions, which may reflect neonatal risk factors, care practices (e.g., target levels for acceptable oxygen saturation), and differences in the clinical definitions of BPD.[10][11][12]
See also
- Respiratory care
- Pulmonology
- Neonatology
- Nursing
- Respiratory distress syndrome
- Wilson–Mikity syndrome
References
- ↑ Northway Jr, WH; Rosan, RC; Porter, DY (Feb 16, 1967). "Pulmonary disease following respirator therapy of hyaline-membrane disease. Bronchopulmonary dysplasia.". The New England Journal of Medicine. 276 (7): 357–68. doi:10.1056/NEJM196702162760701. PMID 5334613.
- ↑ Sahni, R; Ammari, A; Suri, MS; Milisavljevic, V; Ohira-Kist, K; Wung, JT; Polin, RA (Jan 2005). "Is the new definition of bronchopulmonary dysplasia more useful?". Journal of perinatology : official journal of the California Perinatal Association. 25 (1): 41–6. doi:10.1038/sj.jp.7211210. PMID 15538399.
- ↑ Ehrenkranz, RA; Walsh, MC; Vohr, BR; Jobe, AH; Wright, LL; Fanaroff, AA; Wrage, LA; Poole, K; National Institutes of Child Health and Human Development Neonatal Research, Network (Dec 2005). "Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia". Pediatrics. 116 (6): 1353–60. doi:10.1542/peds.2005-0249. PMID 16322158.
- ↑ Kinsella, JP; Greenough, A; Abman, SH (Apr 29, 2006). "Bronchopulmonary dysplasia". Lancet. 367 (9520): 1421–31. doi:10.1016/S0140-6736(06)68615-7. PMID 16650652.
- ↑ "Bronchopulmonary Dysplasia". Patient.info. Retrieved 2 February 2014.
- ↑ Jobe, AH; Bancalari, E (June 2001). "Bronchopulmonary dysplasia". Am J Respir Crit Care Med. 163 (7): 1726. doi:10.1164/ajrccm.163.7.2011060. PMID 11401896.
- ↑ Gaining & Growing. "Bronchopulmonary dysplasia", Gaining & Growing, March 20, 2007. (Retrieved June 12, 2008.)
- ↑ Doyle, LW; Ehrenkranz, RA; Halliday, HL (May 13, 2014). "Early (< 8 days) postnatal corticosteroids for preventing chronic lung disease in preterm infants.". The Cochrane database of systematic reviews. 5: CD001146. doi:10.1002/14651858.CD001146.pub4. PMID 24825456.
- ↑ Doyle, LW; Ehrenkranz, RA; Halliday, HL (May 13, 2014). "Late (> 7 days) postnatal corticosteroids for chronic lung disease in preterm infants.". The Cochrane database of systematic reviews. 5: CD001145. doi:10.1002/14651858.CD001145.pub3. PMID 24825542.
- ↑ Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR; et al. (2007). "Trends in neonatal morbidity and mortality for very low birthweight infants". Am J Obstet Gynecol. 196 (2): 147.e1–8. doi:10.1016/j.ajog.2006.09.014. PMID 17306659.
- ↑ Van Marter LJ, Allred EN, Pagano M, Sanocka U, Parad R, Moore M; et al. (2000). "Do clinical markers of barotrauma and oxygen toxicity explain interhospital variation in rates of chronic lung disease? The Neonatology Committee for the Developmental Network". Pediatrics. 105 (6): 1194–201. doi:10.1542/peds.105.6.1194. PMID 10835057.
- ↑ Ellsbury DL, Acarregui MJ, McGuinness GA, Eastman DL, Klein JM (2004). "Controversy surrounding the use of home oxygen for premature infants with bronchopulmonary dysplasia". J Perinatol. 24 (1): 36–40. doi:10.1038/sj.jp.7211012. PMID 14726936.
Further reading
- Bhandari, A; Bhandari, V (Jan 2007). "Bronchopulmonary dysplasia: an update" (PDF). Indian journal of pediatrics. 74 (1): 73–7. doi:10.1007/s12098-007-0032-z. PMID 17264460.
- Bronchopulmonary Dysplasia on National Institutes of Health