Asystole
| Asystole | |
|---|---|
|
A rhythm strip showing two beats of normal sinus rhythm followed by an atrial beat and asystole. | |
| Classification and external resources | |
| Pronunciation | /əˈsɪstəliː/ |
| Specialty | cardiology |
| ICD-10 | I46.0 |
| ICD-9-CM | 427.5 |
Asystole, also known as flatline, is a state of no electrical activity from the heart and therefore no blood flow. It results in cardiac arrest. Asystole is found initially in about 28% of people in cardiac arrest.[1]
Asystole is treated by cardiopulmonary resuscitation (CPR) combined with an intravenous vasopressor such as epinephrine (aka adrenaline). Sometimes an underlying reversible cause can be detected and treated (the so-called 'Hs and Ts', an example of which is hypokalaemia). Several interventions previously recommended—such as defibrillation (known to be ineffective on asystole, but previously performed in case the rhythm was actually very fine ventricular fibrillation) and intravenous atropine—are no longer part of the routine protocols recommended by most major international bodies.[2] Asystole may be treated with 1 mg epinephrine by IV every 3–5 minutes as needed. Vasopressin 40 units by IV every 3–5 minutes may be used in place of the first and/or second doses of epinephrine, but doing so does not enhance outcomes.
Survival rates in a cardiac arrest patient with asystole are much lower than a patient with a rhythm amenable to defibrillation; asystole is itself not a "shockable" rhythm. Out-of-hospital survival rates (even with emergency intervention) are less than 2 percent.[3]
Cause
Possible underlying causes include the Hs and Ts.[4][5][6]
- Hypovolemia
- Hypoxia
- Hydrogen ions (acidosis)
- Hypothermia
- Hyperkalemia or Hypokalemia
- Hypoglycemia
- Tablets or Toxins (drug overdose)
- Electric shock
- Tachycardia
- Cardiac Tamponade
- Tension pneumothorax
- Thrombosis (myocardial infarction or pulmonary embolism)
- Trauma (hypovolemia from blood loss)
While the heart is asystolic, there is no blood flow to the brain unless CPR or internal cardiac massage (when the chest is opened and the heart is manually compressed) is performed, and even then it is a small amount. After many emergency treatments have been applied but the heart is still unresponsive, it is time to consider pronouncing the patient dead. Even in the rare case that a rhythm reappears, if asystole has persisted for fifteen minutes or more, the brain will have been deprived of oxygen long enough to cause brain death.
-
ECG lead showing asystole (flatline)
-

Asystole
-
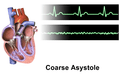
Asystole coarse
See also
References
- ↑ Baldzizhar, A; Manuylova, E; Marchenko, R; Kryvalap, Y; Carey, MG (September 2016). "Ventricular Tachycardias: Characteristics and Management.". Critical care nursing clinics of North America. 28 (3): 317–29. PMID 27484660.
- ↑ AHA Cardiac Recussitation Guidelines, 2010: http://circ.ahajournals.org/cgi/content/full/122/18_suppl_3/S729
- ↑ http://journals.lww.com/surveyanesthesiology/Citation/2008/10000/Medical_Futility_in_Asystolic_Out_of_Hospital.44.aspx
- ↑ Mazur G (2004). ACLS: Principles And Practice. Dallas: American Heart Assn. pp. 71–87. ISBN 0-87493-341-2.
- ↑ Barnes TG, Cummins RO, Field J, Hazinski MF (2003). ACLS for experienced providers. Dallas: American Heart Assn. pp. 3–5. ISBN 0-87493-424-9.
- ↑ ECC Committee, Subcommittees and Task Forces of the American Heart Association (Dec 2005). "2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care - Part 7.2: Management of Cardiac Arrest.". Circulation. 112 (24 Suppl): IV1–203 (7.2 IV58–66). doi:10.1161/CIRCULATIONAHA.105.166550. PMID 16314375.