Artificial organ
An artificial organ is a man-made device that is implanted or integrated into a human — interfacing with living tissue — to replace a natural organ, for the purpose of duplicating or augmenting a specific function or a group of related functions so the patient may return to a normal life as soon as possible. The replaced function doesn't necessarily have to be related to life support, but it often is. For example, replacement bones and joints, such as those found in hip replacements, could also be considered artificial organs.[1][2][3]
Implied by this definition is the fact that the device must not be continuously tethered to a stationary power supply or other stationary resources such as filters or chemical processing units. (Periodic rapid recharging of batteries, refilling of chemicals, and/or cleaning/replacing of filters would exclude a device from being called an artificial organ.)[4] Thus a dialysis machine, while a very successful and critically important life support device that almost completely replaces the duties of a kidney, is not an artificial organ.
Purpose
Reasons to construct and install an artificial organ, an extremely research-intensive and expensive process initially, which may entail many years of ongoing maintenance services not needed by a natural organ, might include:[1][4][5][6]
- providing life support to prevent imminent death while awaiting a transplant (e.g. artificial heart);
- dramatically improving the patient's ability for self care (e.g. artificial limb);
- improving the patient's ability to interact socially (e.g. cochlear implant); or
- improving a patient's quality of life through cosmetic restoration after cancer surgery or an accident.
The use of any artificial organ by humans is almost always preceded by extensive experiments with animals.[7][8] Initial testing in humans is frequently limited to those either already facing death or who have exhausted every other treatment possibility.
Examples
Artificial limbs

Artificial arms and legs, or prosthetics, are intended to restore a degree of normal function to amputees. Mechanical devices that allow amputees to walk again or continue to use two hands have probably been in use since ancient times,[9] the most notable one being the simple peg leg. Since then, the development of artificial limbs has progressed rapidly. New plastics and other materials, such as carbon fiber have allowed artificial limbs to become stronger and lighter, limiting the amount of extra energy necessary to operate the limb. Additional materials have allowed artificial limbs to look much more realistic.[10] Prostheses can roughly be categorized as upper- and lower-extremity and can take many shapes and sizes.
New advances in artificial limbs include additional levels of integration with the human body. Electrodes can be placed into nervous tissue, and the body can be trained to control the prosthesis. This technology has been used in both animals and humans.[11] The prosthetic can be controlled by the brain using a direct implant or implant into various muscles.[12]
Bladder
The two main methods for replacing bladder function involve either redirecting urine flow or replacing the bladder in situ.[13] Standard methods for replacing the bladder involve fashioning a bladder-like pouch from intestinal tissue.[13] An alternative emerging method involves growing a bladder from cells taken from the patient and allowed to grow on a bladder-shaped scaffold.[14]
Brain
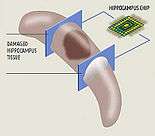
Neural prostheses are a series of devices that can substitute a motor, sensory or cognitive modality that might have been damaged as a result of an injury or a disease.
Neurostimulators, including deep brain stimulators, send electrical impulses to the brain in order to treat neurological and movement disorders, including Parkinson's disease, epilepsy, treatment resistant depression, and other conditions such as urinary incontinence. Rather than replacing existing neural networks to restore function, these devices often serve by disrupting the output of existing malfunctioning nerve centers to eliminate symptoms.[15][16][17]
Corpora cavernosa
To treat erectile dysfunction, both corpora cavernosa can be irreversibly surgically replaced with manually inflatable penile implants. This is a drastic therapeutic surgery meant only for men who suffer from complete impotence who have resisted all other treatment approaches. An implanted pump in the (groin) or (scrotum) can be manipulated by hand to fill these artificial cylinders, normally sized to be direct replacements for the natural corpora cavernosa, from an implanted reservoir in order to achieve an erection.[18]
Ear
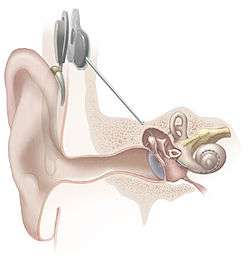
In cases when a person is profoundly deaf or severely hard of hearing in both ears, a cochlear implant may be surgically implanted. Cochlear implants bypass most of the peripheral auditory system to provides a sense of sound via a microphone and some electronics that reside outside the skin, generally behind the ear. The external components transmit a signal to an array of electrodes placed in the cochlea, which in turn stimulates the cochlear nerve.[19]
In the case of an outer ear trauma, a craniofacial prosthesis may be necessary.
Eye

The most successful function-replacing artificial eye so far is actually an external miniature digital camera with a remote unidirectional electronic interface implanted on the retina, optic nerve, or other related locations inside the brain. The present state of the art yields only partial functionality, such as recognizing levels of brightness, swatches of color, and/or basic geometric shapes, proving the concept's potential.[20]
Various researchers have demonstrated that the retina performs strategic image preprocessing for the brain. The problem of creating a completely functional artificial electronic eye is even more complex. Advances towards tackling the complexity of the artificial connection to the retina, optic nerve, or related brain areas, combined with ongoing advances in computer science, are expected to dramatically improve the performance of this technology.
Heart
Cardiovascular-related artificial organs are implanted in cases where the heart, its valves, or another part of the circulatory system is in disorder. The artificial heart is typically used to bridge the time to heart transplantation, or to permanently replace the heart in case heart transplantation is impossible. Artificial pacemakers represent another cardiovascular device which can be implanted to either intermittently augment (defibrillator mode), continuously augment, or completely bypass the natural living cardiac pacemaker as needed. Ventricular assist devices are another alternative, acting as mechanical circulatory devices that partially or completely replace the function of a failing heart, without the removal of the heart itself.[21]
Besides these, lab-grown hearts are also being researched.
Liver
HepaLife is developing a bioartificial liver device intended for the treatment of liver failure using stem cells. The artificial liver is designed to serve as a supportive device, either allowing the liver to regenerate upon failure, or to bridge the patient's liver functions until transplant is available.[22] It is only made possible by the fact that it uses real liver cells (hepatocytes), and even then, it is not a permanent substitute.
Researchers from Japan found that a mixture of human liver precursor cells (differentiated from human induced pluripotent stem cells [iPSCs]) and two other cell types can spontaneously form three-dimensional structures dubbed “liver buds.”[23]
Lungs

With some almost fully functional, artificial lungs promise to be a great success in near future.[24] An Ann Arbor company MC3 is currently working on this type of medical device.
Extracorporeal membrane oxygenation (ECMO) can be used to take significant load off of the native lung tissue and heart. In ECMO, a one or more catheters are placed into the patient and a pump is used to flow blood over hollow membrane fibers, which exchange oxygen and carbon dioxide with the blood. Similar to ECMO, Extracorporeal CO2 Removal (ECCO2R) has a similar set-up, but mainly benefits the patient through carbon dioxide removal, rather than oxygenation, with the goal of allowing the lungs to relax and heal.[25]
Ovaries
Reproductive age patients who develop cancer often receive chemotherapy or radiation therapy which damages oocytes and leads to early menopause. An artificial human ovary has been developed at Brown University[26] with self-assembled microtissues created using novel 3-D petri dish technology. The artificial ovary will be used for the purpose of in vitro maturation of immature oocytes and the development of a system to study the effect of environmental toxins on folliculogenesis.
Pancreas
An artificial pancreas is used to substitute endocrine functionality of a healthy pancreas for diabetic and other patients who require it. It can be used to improve insulin replacement therapy until glycemic control is practically normal as evident by the avoidance of the complications of hyperglycemia, and it can also ease the burden of therapy for the insulin-dependent. Approaches include using an insulin pump under closed loop control, developing a bio-artificial pancreas consisting of a biocompatible sheet of encapsulated beta cells, or using gene therapy.[27][28]
Thymus
An implantable machine that performs the function of a thymus does not exist. However, researchers have been able to grow a thymus from reprogrammed fibroblasts. They expressed hope that the approach could one day replace or supplement neonatal thymus transplantation.[29]
Trachea
Surgeons in Sweden performed the first implantation of a synthetic trachea in July 2011, for a 36-year-old patient who was suffering from cancer. Stem cells taken from the patient's hip were treated with growth factors and incubated on a plastic replica of his natural trachea.[30]
Enhancement
It is also possible to construct and install an artificial organ to give its possessor abilities which are not naturally occurring. Research is proceeding in areas of vision, memory, and information processing. Some current research focuses on restoring short-term memory in accident victims and long-term memory in dementia patients.
One area of success was achieved when Kevin Warwick carried out a series of experiments extending his nervous system over the internet to control a robotic hand and the first direct electronic communication between the nervous systems of two humans.[31]
This might also include the existing practice of implanting subcutaneous chips for identification and location purposes (ex. RFID tags).
Microchips
Scientists are developing palm-sized mock human organs, designed to test drugs and help understand the basic function of healthy or diseased organs. Researchers are hopeful this technology may speed up drug development and make it less expensive.[32]
See also
- Artificial bone, skin, uterus, kidney
- Biomechatronics
- Biomedical Engineering
- Decellularization
- Organ transplant
- Organ culture
- Tissue scaffold
References
- 1 2 Catapano, G.; Verkerke, G.J. (2012). "Chapter 2: Artificial Organs". In Abu-Faraj, Z.O. Handbook of Research on Biomedical Engineering Education and Advanced Bioengineering Learning: Interdisciplinary Concepts - Volume 1. Hershey, PA: Medical Information Science Reference. pp. 60–95. ISBN 9781466601239. Retrieved 16 March 2016.
- ↑ Gebelein, C.G. (1984). "Chapter 1: The Basics of Artificial Organs". In Gebelein, C.G. Polymeric Materials and Artificial Organs (PDF). Washington, DC: American Chemical Society. pp. 1–11. doi:10.1021/bk-1984-0256.ch001. ISBN 9780841208544. Retrieved 16 March 2016.
- ↑ "Artificial Organs". Reference.MD. RES, Inc. 6 June 2012. Retrieved 16 March 2016.
- 1 2 Tang, R. (1998). "Artificial Organs". Bios. 69 (3): 119–122. JSTOR 4608470.
- ↑ Fountain, H. (15 September 2012). "A First: Organs Tailor-Made With Body's Own Cells". The New York Times. The New York Times Company. Retrieved 16 March 2016.
- ↑ Mussivand, T.; Kung, R.T.V.; McCarthy, P.M.; et al. (1997). "Cost Effectiveness of Artificial Organ Technologies Versus Conventional Therapy". ASAIO Journal. 43 (3): 230–236. doi:10.1097/00002480-199743030-00021. PMID 9152498. Retrieved 16 March 2016.
- ↑ "Why are animals used for testing medical products?". FDA.org. Food and Drug Administration. 4 March 2016. Retrieved 16 March 2016.
- ↑ Giardino, R.; Fini, M.; Orienti, L. (1997). "Laboratory animals for artificial organ evaluation". International Journal of Artificial Organs. 20 (2): 76–80. PMID 9093884.
- ↑ Finch, J. (February 2011). "The Art of Medicine: The Ancient Origins of Prosthetic Medicine" (PDF). The Lancet. 377 (9765): 348–349. doi:10.1016/s0140-6736(11)60190-6. PMID 21341402. Retrieved 16 March 2016.
- ↑ "Artificial Limb". How Products Are Made. Advameg, Inc. Retrieved 16 March 2016.
- ↑ http://motorlab.neurobio.pitt.edu/multimedia.php
- ↑ http://www.ric.org/conditions/prosthetics-orthotics/bionic/
- 1 2 "Treatments & Procedures", Urinary Reconstruction and Diversion, Cleveland Clinic, 2009, retrieved 2013-03-22
- ↑ Smith, Stephanie (2006), "Doctors grow organs from patients' own cells", CNN.com, CNN, retrieved 2013-03-22
- ↑ Wong, J.Y.; Bronzino, J.D.; Peterson, D.R., eds. (2012). Biomaterials: Principles and Practices. Boca Raton, FL: CRC Press. p. 281. ISBN 9781439872512. Retrieved 16 March 2016.
- ↑ "Download Product Code Classification Files". FDA.org/medicaldevices. Food and Drug Administration. 4 November 2014. Retrieved 16 March 2016.
Relevant info in the foiclass.zip file.
- ↑ McLatchie, G.; Borley, N.; Chikwe, J., eds. (2013). Oxford Handbook of Clinical Surgery. Oxford, UK: OUP Oxford. p. 794. ISBN 9780199699476. Retrieved 16 March 2016.
- ↑ Simmons, M.; Montague D.K. (2008). "Penile prosthesis implantation: Past, present, and future". International Journal of Impotence Research. 20 (5): 437–444. doi:10.1038/ijir.2008.11. PMID 18385678.
- ↑ "Cochlear Implants". NIH Publication No. 11-4798. National Institute on Deafness and Other Communication Disorders. February 2016. Retrieved 16 March 2016.
- ↑ Geary, J. (2002). The Body Electric. Rutgers University Press. p. 214. ISBN 9780813531946. Retrieved 16 March 2016.
- ↑ Birks, E.J.; Tansley, P.D.; Hardy, J.; et al. (2006). "Left Ventricular Assist Device and Drug Therapy for the Reversal of Heart Failure". New England Journal of Medicine. 355 (18): 1873–1884. doi:10.1056/NEJMoa053063. PMID 17079761.
- ↑ HepaLife - Artificial Liver
- ↑ Takanori Takebe, Keisuke Sekine, Masahiro Enomura, et al. & Hideki Taniguchi (2013) Vascularized and functional human liver from an iPSC-derived organ bud transplant. Nature doi:10.1038/nature12271
- ↑ Ota, K. (2010). Advances in artificial lungs. Journal of Artificial Organs, 13(1), 13-16.
- ↑ Terragni PP, Birocco A, Faggiano C, Ranieri VM (2010). "Extracorporeal CO2 removal". Contrib Nephrol. 165: 185–96. doi:10.1159/000313758. PMID 20427969.
- ↑ Krotz S, Robins J, Moore R, Steinhoff MM, Morgan J, Carson S. Model Artificial Human Ovary by Pre-Fabricated Cellular Self-Assembly. 64th Annual Meeting of the American Society for Reproductive Medicine, San Francisco, CA 2008
- ↑ "Artificial Pancrease". JDRF. Retrieved 16 March 2016.
- ↑ "Collaborative Efforts Key to Catalyzing Creation of an Artificial Pancreas". National Institute of Diabetes and Digestive and Kidney Diseases. 1 March 2014. Retrieved 16 March 2016.
- ↑ Bredenkamp, N.; Ulyanchenko, S.; o’Neill, K. E.; Manley, N. R.; Vaidya, H. J.; Blackburn, C. C. (2014). "An organized and functional thymus generated from FOXN1-reprogrammed fibroblasts". Nature Cell Biology. 16: 902–908. doi:10.1038/ncb3023.
- ↑ "Cancer Patient Gets First Totally Artificial Windpipe". 2011-07-08. Archived from the original on 12 July 2011. Retrieved 2011-08-07.
- ↑ Warwick K, Gasson M, Hutt B, Goodhew I, Kyberd P, Schulzrinne H, Wu X (2004). "Thought Communication and Control: A First Step using Radiotelegraphy". IEE Proceedings on Communications. 151 (3): 185–189. doi:10.1049/ip-com:20040409.
- ↑ Richard Harris (2 January 2015). "Researchers Create Artificial Organs On Microchips". NPR.
Further reading
- Tran, Jasper (2015). "To Bioprint or Not to Bioprint". North Carolina Journal of Law and Technology. 17: 123–78.
- Yunying Liu, Ru Yang, Zuping He and Wei-Qiang Gao (2013), Generation of functional organs from stem cells. Cell Regeneration, 2:1 doi:10.1186/2045-9769-2-1
- Artificial Organs, official peer-reviewed journal of the International Federation for Artificial Organs
- Hardware Models of Hippocampus: Toward Brain Implants as Neural Prostheses for Memory Loss
- Adaptive Optoelectronic Eye: Hybrid Sensor/Processor Architecture