Anorexia nervosa
| Anorexia nervosa | |
|---|---|
|
"Miss A—" pictured in 1866 and in 1870 after treatment. She was one of the earliest case studies of anorexia. From the published medical papers of Sir William Gull | |
| Classification and external resources | |
| Specialty | Psychiatry |
| ICD-10 | F50.0-F50.1 |
| ICD-9-CM | 307.1 |
| OMIM | 606788 |
| DiseasesDB | 749 |
| MedlinePlus | 000362 |
| eMedicine | emerg/34 med/144 |
| Patient UK | Anorexia nervosa |
| MeSH | D000856 |
Anorexia nervosa, often referred to simply as anorexia,[1] is an eating disorder characterized by a low weight, fear of gaining weight, a strong desire to be thin, and food restriction.[2] Many people with anorexia see themselves as overweight even though they are in fact underweight.[2][3] If asked they usually deny they have a problem with low weight.[4] Often they weigh themselves frequently, eat only small amounts, and only eat certain foods. Some will exercise excessively, force themselves to vomit, or use laxatives to produce weight loss. Complications may include osteoporosis, infertility and heart damage, among others.[2] Women will often stop having menstrual periods.[4]
The cause is not known. There appear to be some genetic components with identical twins more often affected than non-identical twins.[3] Cultural factors also appear to play a role with societies that value thinness having higher rates of disease.[4] Additionally, it occurs more commonly among those involved in activities that value thinness such as high-level athletics, modelling, and dancing.[4][5] Anorexia often begins following a major life change or stress-inducing event. The diagnosis requires a significantly low weight. The severity of disease is based on body mass index (BMI) in adults with mild disease having a BMI of greater than 17, moderate a BMI of 16 to 17, severe a BMI of 15 to 16, and extreme a BMI less than 15. In children a BMI for age percentile of less than the 5th percentile is often used.[4]
Treatment of anorexia involves restoring a healthy weight, treating the underlying psychological problems, and addressing behaviors that promote the problem. While medications do not help with weight gain, they may be used to help with associated anxiety or depression.[2] A number of types of therapy may be useful including an approach where parents assume responsibility for feeding their child, known as Maudsley family therapy and cognitive behavioral therapy.[2][6] Sometimes people require admission to hospital to restore weight.[7] Evidence for benefit from nasogastric tube feeding; however, is unclear.[8] Some people will just have a single episode and recover while others may have many episodes over years.[7] Many complications improve or resolve with regaining of weight.[7]
Globally, anorexia is estimated to affect two million people as of 2013.[9] It is estimated to occur in 0.9% to 4.3% of women and 0.2% to 0.3% of men in Western countries at some point in their life.[10] About 0.4% of young females are affected in a given year and it is estimated to occur ten times less commonly in males.[4][10] Rates in most of the developing world are unclear.[4] Often it begins during the teen years or young adulthood.[2] While anorexia became more commonly diagnosed during the 20th century it is unclear if this was due to an increase in its frequency or simply better diagnosis.[3] In 2013 it directly resulted in about 600 deaths globally up from 400 deaths in 1990.[11] Eating disorders also increase a person's risk of death from a wide range of other causes including suicide.[2][10] About 5% of people with anorexia die from complications over a ten-year period, a nearly 6 times increased risk.[4][12] The term anorexia nervosa was first used in 1873 by William Gull to describe this condition.[13]

Signs and symptoms
.jpg)
Anorexia nervosa is an eating disorder characterized by attempts to lose weight, to the point of starvation. A person with anorexia nervosa may exhibit a number of signs and symptoms, the type and severity of which may vary and may be present but not readily apparent.[14]
Anorexia nervosa, and the associated malnutrition that results from self-imposed starvation, can cause complications in every major organ system in the body.[15] Hypokalaemia, a drop in the level of potassium in the blood, is a sign of anorexia nervosa.[16][17] A significant drop in potassium can cause abnormal heart rhythms, constipation, fatigue, muscle damage and paralysis.[18] Some individuals may lack awareness that they are ill.
Symptoms may include:
- A low body mass index for ones age, height and weight.
- Amenorrhea, a symptom that occurs after prolonged weight loss; causes menses to stop, hair becomes brittle, and skin becomes yellow and unhealthy.
- Fear of even the slightest weight gain; taking all precautionary measures to avoid weight gain or becoming "overweight".[19]
- Rapid, continuous weight loss.[20]
- Lanugo: soft, fine hair growing over the face and body.[17]
- An Obsession with counting calories and monitoring fat contents of food.
- Preoccupation with food, recipes, or cooking; may cook elaborate dinners for others, but not eat the food themselves or consume a very small portion.
- Food restrictions despite being underweight or at a healthy weight.
- Food rituals, such as cutting food into tiny pieces, refusing to eat around others and hiding or discarding of food.
- Purging: May use laxatives, diet pills, ipecac syrup, or water pills to flush food out of there system after eating or may engage in self-induced vomiting though this is a more common symptom of bulimia.
- Excessive exercise[21] including micro-exercising, for example making small persistent movements of fingers or toes.[22]
- Perception of self as overweight, even though they might not be.
- Intolerance to cold and frequent complaints of being cold; body temperature may lower (hypothermia) in an effort to conserve energy due to malnutrition.[23]
- Hypotension or orthostatic hypotension.
- Bradycardia or tachycardia.
- Depression, anxiety disorders and insomnia.
- Solitude: may avoid friends and family and become more withdrawn and secretive.
- Abdominal distension.
- Halitosis (from vomiting or starvation-induced ketosis).
- Dry hair and skin, as well as hair thinning.
- Chronic fatigue.[19]
- Rapid mood swings.
- Being protective of ones social media accounts due to eating disorder content.
- Having feet discoloration causing an orange appearance.
- Having severe muscle tension + aches and pains.
- Seeming on edge more often than usual.
- Having teary eyes and suicidal tendencies.
- Evidence/habits of self harming or self loathing.
- Admiration of thinner people.
Associated problems
Other psychological issues may factor into anorexia nervosa; some fulfill the criteria for a separate Axis I diagnosis or a personality disorder which is coded Axis II and thus are considered comorbid to the diagnosed eating disorder. Some people have a previous disorder which may increase their vulnerability to developing an eating disorder and some develop them afterwards. The presence of Axis I or Axis II psychiatric comorbidity has been shown to affect the severity and type of anorexia nervosa symptoms in both adolescents and adults.
Obsessive-compulsive disorder (OCD) and obsessive-compulsive personality disorder (OCPD) are highly comorbid with AN, particularly the restrictive subtype.[24] Obsessive-compulsive personality disorder is linked with more severe symptomatology and worse prognosis.[25] The causality between personality disorders and eating disorders has yet to be fully established. Other comorbid conditions include depression,[26] alcoholism,[27] borderline and other personality disorders,[28][29] anxiety disorders,[30] attention deficit hyperactivity disorder,[31] and body dysmorphic disorder (BDD).[32] Depression and anxiety are the most common comorbidities,[33] and depression is associated with a worse outcome.[33]
Autism spectrum disorders occur more commonly among people with eating disorders than in the general population.[34] Zucker et al. (2007) proposed that conditions on the autism spectrum make up the cognitive endophenotype underlying anorexia nervosa and appealed for increased interdisciplinary collaboration.[35]
Causes
There is evidence for biological, psychological, developmental, and sociocultural risk factors, but the exact cause of eating disorders is unknown.[36]
Biological
- Genetics: anorexia nervosa is highly heritable.[36] Twin studies have shown a heritability rate of between 28 and 58%.[37] Association studies have been performed, studying 128 different polymorphisms related to 43 genes including genes involved in regulation of eating behavior, motivation and reward mechanics, personality traits and emotion. Consistent associations have been identified for polymorphisms associated with agouti-related peptide, brain derived neurotrophic factor, catechol-o-methyl transferase, SK3 and opioid receptor delta-1.[38] Epigenetic modifications, such as DNA methylation, may contribute to the development or maintenance of anorexia nervosa, though clinical research in this area is in its infancy.[39]
- Obstetric complications: prenatal and perinatal complications may factor into the development of anorexia nervosa, such as maternal anemia, diabetes mellitus, preeclampsia, placental infarction, and neonatal cardiac abnormalities. Neonatal complications may also have an influence on harm avoidance, one of the personality traits associated with the development of AN.
- Neuroendocrine dysregulation: altered signalling of peptides that facilitate communication between the gut, brain and adipose tissue, such as ghrelin, leptin, neuropeptide Y and orexin, may contribute to the pathogenesis of anorexia nervosa by disrupting regulation of hunger and satiety.[40][41]
- Gastrointestinal diseases: people with gastrointestinal disorders may be more risk of developing disorders eating practices than the general population, principally restrictive eating disturbances.[42] An association of anorexia nervosa with celiac disease has been found.[43] The role that gastrointestinal symptoms play in the development of eating disorders seems rather complex. Some authors report that unresolved symptoms prior to gastrointestinal disease diagnosis may create a food aversion in these persons, causing alterations to their eating patterns. Other authors report that greater symptoms throughout their diagnosis led to greater risk. It has been documented that some people with celiac disease, irritable bowel syndrome or inflammatory bowel disease who are not conscious about the importance of strictly following their diet, choose to consume their trigger foods to promote weight loss. On the other hand, individuals with good dietary management may develop anxiety, food aversion and eating disorders because of concerns around cross contamination of their foods.[42] Some authors suggest that medical professionals should evaluate the presence of an unrecognized celiac disease in all people with eating disorder, especially if they present any gastrointestinal symptom (such as decreased appetite, abdominal pain, bloating, distension, vomiting, diarrhea or constipation), weight loss, or growth failure; and also routinely ask celiac patients about weight or body shape concerns, dieting or vomiting for weight control, to evaluate the possible presence of eating disorders,[43] specially in women.[44]
Studies have hypothesized the continuance of disordered eating patterns may be epiphenomena of starvation. The results of the Minnesota Starvation Experiment showed normal controls exhibit many of the behavioral patterns of anorexia nervosa (AN) when subjected to starvation. This may be due to the numerous changes in the neuroendocrine system, which results in a self-perpetuating cycle.[45][46][47]
Another hypothesis is that anorexia nervosa is more likely to occur in populations in which obesity is more prevalent, and results from a sexually selected evolutionary drive to appear youthful in populations in which size becomes the primary indicator of age.[48]
Anorexia nervosa is more likely to occur in a person's pubertal years. Some explanatory hypotheses for the rising prevalence of eating disorders in adolescence are "increase of adipose tissue in girls, hormonal changes of puberty, societal expectations of increased independence and autonomy that are particularly difficult for anorexic adolescents to meet; [and] increased influence of the peer group and its values." [49]
Psychological
Early theories of the cause of anorexia linked it to childhood sexual abuse or dysfunctional families;[50][51] evidence is conflicting, and well-designed research is needed.[36] The fear of food is known as sitiophobia,[52] cibophobia,[53] or sitophobia and is part of the differential diagnosis.[54][55] Other psychological causes of Anorexia includes low self-esteem, feeling like there is lack of control, depression, anxiety, and loneliness.[56] Peer pressure and constant pressure media and others around can lead to low self-esteem and other psychological symptoms and causes eating disorders like Anorexia.[57]
Sociological
Anorexia nervosa has been increasingly diagnosed since 1950;[58] the increase has been linked to vulnerability and internalization of body ideals.[49] People in professions where there is a particular social pressure to be thin (such as models and dancers) were more likely to develop anorexia, and those with anorexia have much higher contact with cultural sources that promote weight loss. This trend can also be observed for people who partake in certain sports, such as jockeys and wrestlers.[59] There is a higher incidence and prevalence of anorexia nervosa in sports with an emphasis on aesthetics, where low body fat is advantageous, and sports in which one has to make weight for competition.[60] Family dynamics can play big part in the cause of anorexia.[61] When there is a constant pressure from people to be thin, teasing, bullying can cause low self-esteem and other psychological symptoms.[56]
Media effects
Constant exposure to media that presents body ideals may constitute a risk factor for body dissatisfaction and anorexia nervosa. The cultural ideal for body shape for men versus women continues to favor slender women and athletic, V-shaped muscular men. A 2002 review found that, of the magazines most popular among people aged 18 to 24 years, those read by men, unlike those read by women, were more likely to feature ads and articles on shape than on diet.[62] Body dissatisfaction and internalization of body ideals are risk factors for anorexia nervosa that threaten the health of both male and female populations.
Websites that stress the importance of attainment of body ideals extol and promote anorexia nervosa through the use of religious metaphors, lifestyle descriptions, "thinspiration" or "fitspiration" (inspirational photo galleries and quotes that aim to serve as motivators for attainment of body ideals).[63] Pro-anorexia websites reinforce internalization of body ideals and the importance of their attainment.[63]
The media gives men and women a false view of what people truly look like. In magazines, movies and even on billboards most of the actors/models are photoshopped in multiple ways. People then strive to look like these "perfect" role models when in reality they aren't any where near perfection themselves.[64]
Mechanisms
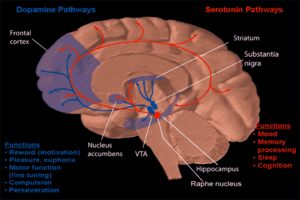
- Serotonin dysregulation: brain imaging studies implicate alterations of 5-HT1A and 5-HT2A receptors and the 5-HT transporter.[36] Alterations of these circuits may affect mood and impulse control as well as the motivating and hedonic aspects of feeding behavior.[65] Starvation has been hypothesized to be a response to these effects, as it is known to lower tryptophan and steroid hormone metabolism, which might reduce serotonin levels at these critical sites and ward off anxiety.[65]
- Addiction to the chemicals released in the brain during starving and physical activity:[66][67] people affected with anorexia often report getting some sort of high from not eating. The effect of food restriction and intense activity causes symptoms similar to anorexia in female rats,[66] though it is not explained why this addiction affects only females.
- Resting state fMRI has identified the insular cortex and corticolimbic circuitry as likely brain areas responsible for the symptomology of anorexia nervosa.[68]
Diagnosis
A diagnostic assessment includes the person's current circumstances, biographical history, current symptoms, and family history. The assessment also includes a mental state examination, which is an assessment of the person's current mood and thought content, focusing on views on weight and patterns of eating.
DSM-5
Anorexia nervosa is classified under the Feeding and Eating Disorders in the latest revision of the Diagnostic and Statistical Manual of Mental Disorders (DSM 5).
Relative to the previous version of the DSM (DSM-IV-TR), the 2013 revision (DSM5) reflects changes in the criteria for anorexia nervosa, most notably that of the amenorrhea criterion being removed.[7][69] Amenorrhea was removed for several reasons: it does not apply to males, it is not applicable for females before or after the age of menstruation or taking birth control pills, and some women who meet the other criteria for AN still report some menstrual activity.[7]
Subtypes
There are two subtypes of AN:[15][70]
- Binge-eating/purging type: the individual utilizes binge eating or displays purging behavior as a means for losing weight.[70] It is different from bulimia nervosa in terms of the individual's weight. An individual with binge-eating/purging type anorexia does not maintain a healthy or normal weight but is significantly underweight. People with bulimia nervosa on the other hand can sometimes be overweight.[19]
- Restricting type: the individual uses restricting food intake, fasting, diet pills, or exercise as a means for losing weight;[15] they may exercise excessively to keep off weight or prevent weight gain, and some individuals eat only enough to stay alive.[15][19]
Levels of severity
Body mass index (BMI) is used by the DSM-5 as an indicator of the level of severity of anorexia nervosa. The DSM-5 states these as follows:[71]
- Mild: BMI of greater than 17
- Moderate: BMI of 16–16.99
- Severe: BMI of 15–15.99
- Extreme: BMI of less than 15
Investigations
Medical tests to check for signs of physical deterioration in anorexia nervosa may be performed by a general physician or psychiatrist, including:
- Complete Blood Count (CBC): a test of the white blood cells, red blood cells and platelets used to assess the presence of various disorders such as leukocytosis, leukopenia, thrombocytosis and anemia which may result from malnutrition.[72]
- Urinalysis: a variety of tests performed on the urine used in the diagnosis of medical disorders, to test for substance abuse, and as an indicator of overall health[73]
- Chem-20: Chem-20 also known as SMA-20 a group of twenty separate chemical tests performed on blood serum. Tests include cholesterol, protein and electrolytes such as potassium, chlorine and sodium and tests specific to liver and kidney function.[74]
- Glucose tolerance test: Oral glucose tolerance test (OGTT) used to assess the body's ability to metabolize glucose. Can be useful in detecting various disorders such as diabetes, an insulinoma, Cushing's Syndrome, hypoglycemia and polycystic ovary syndrome.[75]
- Serum cholinesterase test: a test of liver enzymes (acetylcholinesterase and pseudocholinesterase) useful as a test of liver function and to assess the effects of malnutrition.[76]
- Liver Function Test: A series of tests used to assess liver function some of the tests are also used in the assessment of malnutrition, protein deficiency, kidney function, bleeding disorders, and Crohn's Disease.[77]
- Lh response to GnRH: Luteinizing hormone (Lh) response to gonadotropin-releasing hormone (GnRH): Tests the pituitary glands' response to GnRh a hormone produced in the hypothalamus. Hypogonadism is often seen in anorexia nervosa cases.[16]
- Creatine Kinase Test (CK-Test): measures the circulating blood levels of creatine kinase an enzyme found in the heart (CK-MB), brain (CK-BB) and skeletal muscle (CK-MM).[78]
- Blood urea nitrogen (BUN) test: urea nitrogen is the byproduct of protein metabolism first formed in the liver then removed from the body by the kidneys. The BUN test is primarily used to test kidney function. A low BUN level may indicate the effects of malnutrition.[79]
- BUN-to-creatinine ratio: A BUN to creatinine ratio is used to predict various conditions. A high BUN/creatinine ratio can occur in severe hydration, acute kidney failure, congestive heart failure, and intestinal bleeding. A low BUN/creatinine ratio can indicate a low protein diet, celiac disease, rhabdomyolysis, or cirrhosis of the liver.[80][81]
- Electrocardiogram (EKG or ECG): measures electrical activity of the heart. It can be used to detect various disorders such as hyperkalemia[82]
- Electroencephalogram (EEG): measures the electrical activity of the brain. It can be used to detect abnormalities such as those associated with pituitary tumors.[83]
- Thyroid Screen TSH, t4, t3 :test used to assess thyroid functioning by checking levels of thyroid-stimulating hormone (TSH), thyroxine (T4), and triiodothyronine (T3)[84]
Differential diagnoses
A variety of medical and psychological conditions have been misdiagnosed as anorexia nervosa; in some cases the correct diagnosis was not made for more than ten years.
The distinction between the diagnoses of anorexia nervosa, bulimia nervosa and eating disorder not otherwise specified (EDNOS) is often difficult to make as there is considerable overlap between people diagnosed with these conditions. Seemingly minor changes in a people's overall behavior or attitude can change a diagnosis from anorexia: binge-eating type to bulimia nervosa. A main factor differentiating binge-purge anorexia from bulimia is the gap in physical weight. Someone with bulimia nervosa is ordinarily at a healthy weight, or slightly overweight. Someone with binge-purge anorexia is commonly underweight.[85] People with the binge-purging subtype of AN may be significantly underweight and typically do not binge-eat large amounts of food, yet they purge the small amount of food they eat.[85] In contrast, those with bulimia nervosa tend to be at normal weight or overweight and binge large amounts of food.[85] It is not unusual for a person with an eating disorder to "move through" various diagnoses as their behavior and beliefs change over time.[35]
Treatment
There is no conclusive evidence that any particular treatment for anorexia nervosa works better than others; however, there is enough evidence to suggest that early intervention and treatment are more effective.[86] Treatment for anorexia nervosa tries to address three main areas.
- Restoring the person to a healthy weight;
- Treating the psychological disorders related to the illness;
- Reducing or eliminating behaviours or thoughts that originally led to the disordered eating.[87]
Although restoring the person's weight is the primary task at hand, optimal treatment also includes and monitors behavioral change in the individual as well.[88] There is some evidence that hospitalisation might adversely affect long term outcome.[89]
Psychotherapy for individuals with AN is challenging as they may value being thin and may seek to maintain control and resist change.[90] Some studies demonstrate that family based therapy in adolescents with AN is superior to individual therapy.[91]
Treatment of people with AN is difficult because they are afraid of gaining weight. Initially developing a desire to change may be important.[92]
Diet
Diet is the most essential factor to work on in people with anorexia nervosa, and must be tailored to each person's needs. Food variety is important when establishing meal plans as well as foods that are higher in energy density.[93] People must consume adequate calories, starting slowly, and increasing at a measured pace.[21] Evidence of a role for zinc supplementation during refeeding is unclear.[8]
Therapy
Family-based treatment (FBT) has been shown to be more successful than individual therapy for adolescents with AN.[12][94] Various forms of family-based treatment have been proven to work in the treatment of adolescent AN including conjoint family therapy (CFT), in which the parents and child are seen together by the same therapist, and separated family therapy (SFT) in which the parents and child attend therapy separately with different therapists.[12] Proponents of Family therapy for adolescents with AN assert that it is important to include parents in the adolescent's treatment.[12]
A four- to five-year follow up study of the Maudsley family therapy, an evidence-based manualized model, showed full recovery at rates up to 90%.[95] Although this model is recommended by the NIMH,[96] critics claim that it has the potential to create power struggles in an intimate relationship and may disrupt equal partnerships.[97]
Cognitive behavioral therapy (CBT) is useful in adolescents and adults with anorexia nervosa;[98] acceptance and commitment therapy is a type of CBT, which has shown promise in the treatment of AN.[99] Cognitive remediation therapy (CRT) is used in treating anorexia nervosa.[100]
Medication
Pharmaceuticals have limited benefit for anorexia itself.[101]
Admission to hospital
AN has a high mortality[102] and patients admitted in a severely ill state to medical units are at particularly high risk. Diagnosis can be challenging, risk assessment may not be performed accurately, consent and the need for compulsion may not be assessed appropriately, refeeding syndrome may be missed or poorly treated and the behavioural and family problems in AN may be missed or poorly managed.[103] The MARSIPAN guidelines recommend that medical and psychiatric experts work together in managing severely ill people with AN.[104]
Nutrition
The rate of refeeding can be difficult to establish, because the fear of refeeding syndrome (RFS) can lead to underfeeding. It is thought that RFS, with falling phosphate and potassium levels, is more likely to occur when BMI is very low, and when medical comorbidities such as infection or cardiac failure, are present. In those circumstances, it is recommended to start refeeding slowly but to build up rapidly as long as RFS does not occur. Recommendations on energy requirements vary, from 5-10 kCal/Kg/day in the most medically compromised patients, who appear to have the highest risk of RFS to 1900 Kcal/day[105][106]
Prognosis

AN has the highest mortality rate of any psychological disorder.[12] The mortality rate is 6 to 12 times higher than expected, and the suicide risk is 56 times higher; half of women with AN achieve a full recovery, while an additional 20–30% may partially recover.[12][16] Not all people with anorexia recover completely: about 20% develop anorexia nervosa as a chronic disorder.[86] If anorexia nervosa is not treated, serious complications such as heart conditions[14] and kidney failure can arise and eventually lead to death.[107] The average number of years from onset to remission of AN is seven for women and three for men. After ten to fifteen years, 70% of people no longer meet the diagnostic criteria, but many still continue to have eating-related problems.[108]
Alexithymia influences treatment outcome.[101] Recovery is also viewed on a spectrum rather than black and white. According to the Morgan-Russell criteria, individuals can have a good, intermediate, or poor outcome. Even when a person is classified as having a "good" outcome, weight only has to be within 15% of average, and normal menstruation must be present in females. The good outcome also excludes psychological health. Recovery for people with anorexia nervosa is undeniably positive, but recovery does not mean a return to normal.
Complications
Anorexia nervosa can have serious implications if its duration and severity are significant and if onset occurs before the completion of growth, pubertal maturation, or the attainment of peak bone mass. Complications specific to adolescents and children with anorexia nervosa can include the following: Growth retardation may occur, as height gain may slow and can stop completely with severe weight loss or chronic malnutrition. In such cases, provided that growth potential is preserved, height increase can resume and reach full potential after normal intake is resumed. Height potential is normally preserved if the duration and severity of illness are not significant or if the illness is accompanied with delayed bone age (especially prior to a bone age of approximately 15 years), as hypogonadism may negate the deleterious effects of undernutrition on stature by allowing for a longer duration of growth compared to controls. In such cases, appropriate early treatment can preserve height potential and may even help to increase it in some post-anorexic subjects due to the aforementioned reasons in addition to factors such as long-term reduced estrogen-producing adipose tissue levels compared to premorbid levels. In some cases, especially where onset is pre-pubertal, physical consequences such as stunted growth and pubertal delay are usually fully reversible.[109]
Anorexia nervosa causes alterations in the female reproductive system; significant weight loss, as well as psychological stress and intense exercise, typically results in a cessation of menstruation in women who are past puberty. In patients with anorexia nervosa, there is a reduction of the secretion of gonadotropin releasing hormone in the central nervous system, preventing ovulation.[110] Anorexia nervosa can also result in pubertal delay or arrest. Both height gain and pubertal development are dependent on the release of growth hormone and gonadotrophins (LH and FSH) from the pituitary gland. Suppression of gonadotrophins in people with anorexia nervosa has been documented.[111] Typically, growth hormone (GH) levels are high, but levels of IGF-1, the downstream hormone that should be released in response to GH are low; this indicates a state of “resistance” to GH due to chronic starvation.[112] IGF-1 is necessary for bone formation, and decreased levels in anorexia nervosa contribute to a loss of bone density and potentially contribute to osteopenia or osteoporosis.[112] Anorexia nervosa can also result in reduction of peak bone mass. Buildup of bone is greatest during adolescence, and if onset of anorexia nervosa occurs during this time and stalls puberty, low bone mass may be permanent.[113] Hepatic steatosis, or fatty infiltration of the liver, can also occur, and is an indicator of malnutrition in children.[114] Neurological disorders that may occur as complications include seizures and tremors. Wernicke encephalopathy, which results from vitamin B1 deficiency, has been reported in patients who are extremely malnourished; symptoms include confusion, oculomotor dysfunction, and abnormalities in walking gait.
The most common gastrointestinal complications of anorexia nervosa are delayed stomach emptying and constipation, but also include elevated liver function tests, diarrhea, acute pancreatitis, heartburn, difficulty swallowing, and, rarely, superior mesenteric artery syndrome.[115] Delayed stomach emptying, or gastroparesis, often develops following food restriction and weight loss; the most common symptom is bloating with gas and abdominal distension, and often occurs after eating. Other symptoms of gastroparesis include early satiety, fullness, nausea, and vomiting. The symptoms may inhibit efforts at eating and recovery, but can be managed by limiting high-fiber foods, using liquid nutritional supplements, or using metoclopramide to increase emptying of food from the stomach.[115] Gastroparesis generally resolves when weight is regained.
Cardiac complications
Anorexia nervosa increases the risk of sudden cardiac death, though the precise cause is unknown. Cardiac complications include structural and functional changes to the heart.[116] Some of these cardiovascular changes are mild and are reversible with treatment, while others may be life threatening. Cardiac complications can include arrhythmias, abnormally slow heart beat, low blood pressure, decreased size of the heart muscle, reduced heart volume, mitral valve prolapse, myocardial fibrosis, and pericardial effusion.[116]
Abnormalities in conduction and repolarization of the heart that can result from anorexia nervosa include QT prolongation, increased QT dispersion, conduction delays, and junctional escape rhythms.[116] Electrolyte abnormalities, particularly hypokalemia and hypomagnesemia can cause anomalies in the electrical activity of the heart, and result in life-threatening arrhythmias. Hypokalemia most commonly results in anorexic patients when restricting is accompanied by purging (induced vomiting or laxative use). Hypotension (low blood pressure) is common, and symptoms include fatigue and weakness. Orthostatic hypotension, a marked decrease in blood pressure when standing from a supine position, may also occur. Symptoms include lightheadedness upon standing, weakness, and cognitive impairment, and may result in fainting or near-fainting.[116] Orthostasis in anorexia nervosa indicates worsening cardiac function and may indicate a need for hospitalization.[116] Hypotension and orthostasis generally resolve upon recovery to a normal weight. The weight loss in anorexia nervosa also causes atrophy of cardiac muscle. This leads to decreased ability to pump blood, a reduction in the ability to sustain exercise, a diminished ability to increase blood pressure in response to exercise, and a subjective feeling of fatigue.[117] Some individuals may also have a decrease in cardiac contractility. Cardiac complications can be life-threatening, but the heart muscle generally improves with weight gain, and the heart normalizes in size normalizes over weeks to months, with recovery.[117] Atrophy of the heart muscle is a marker of the severity of the disease, and while it is reversible with treatment and refeeding, it is possible that it may cause permanent, microscopic changes to the heart muscle that increase the risk of sudden cardiac death.[116] Individuals with anorexia nervosa may experience chest pain or palpitations; these can be a result of mitral valve prolapse. Mitral valve prolapse occurs because the size of the heart muscle decreases while the tissue of the mitral valve remains the same size. Studies have shown rates of mitral valve prolapse of around 20 percent in those with anorexia nervosa, while the rate in the general population is estimated at 2-4 percent.[118] It has been suggested that there is an association between mitral valve prolapse and sudden cardiac death, but it has not been proven to be causative, either in patients with anorexia nervosa or in the general population.[116]
Relapse
Relapse occurs in approximately a third of people in hospital, and is greatest in the first six to eighteen months after release from an institution.[119]
Epidemiology
Anorexia is estimated to occur in 0.9% to 4.3% of women and 0.2% to 0.3% of men in Western countries at some point in their life.[10] About 0.4% of young females are affected in a given year and it is estimated to occur three to ten times less commonly in males.[4][10][119] Rates in most of the developing world are unclear.[4] Often it begins during the teen years or young adulthood.[2]
The lifetime rate of atypical anorexia nervosa, a form of ED-NOS in which not all of the diagnostic criteria for AN are met, is much higher, at 5–12%.[120]
While anorexia become more commonly diagnosed during the 20th century it is unclear if this was due to an increase in its frequency or simply better diagnosis.[3] Most studies show that since at least 1970 the incidence of AN in adult women is fairly constant, while there is some indication that the incidence may have been increasing for girls aged between 14 and 20.[121]
Underrepresentation
Eating disorders are less reported in preindustrial, non-westernized countries than in Western countries. In Africa, not including South Africa, the only data presenting information about eating disorders occurs in case reports and isolated studies, not studies investigating prevalence. Data shows in research that in westernized civilizations, ethnic minorities have very similar rates of eating disorders, contrary to the belief that eating disorders predominantly occur in Caucasian people.
Due to different standards of beauty for men and women, men are often not diagnosed as anorexic. Generally men who alter their bodies do so to be lean and muscular rather than thin. In addition, men who might otherwise be diagnosed with anorexia may not meet the DSM IV criteria for BMI since they have muscle weight, but have very little fat.[122] Men and women athletes are often overlooked as anorexic.[122] Research emphasizes the importance to take athletes' diet, weight and symptoms into account when diagnosing anorexia, instead of just looking at weight and BMI. For athletes, ritualized activities such as weigh-ins place emphasis on weight, which may promote the development of eating disorders among them. While women use diet pills, which is an indicator of unhealthy behavior and an eating disorder, men use steroids, which contextualizes the beauty ideals for genders. This also shows men having a preoccupation with their body, which is an indicator of an eating disorder.[36] In a Canadian study, 4% of boys in grade nine used anabolic steroids.[36] Anorexic men are sometimes referred to as manorexic.[123]
History
The term anorexia nervosa was coined in 1873 by Sir William Gull, one of Queen Victoria's personal physicians.[124] The history of anorexia nervosa begins with descriptions of religious fasting dating from the Hellenistic era[125] and continuing into the medieval period. The medieval practice of self-starvation by women, including some young women, in the name of religious piety and purity also concerns anorexia nervosa; it is sometimes referred to as anorexia mirabilis.[126][127]
The earliest medical descriptions of anorexic illnesses are generally credited to English physician Richard Morton in 1689.[125] Case descriptions fitting anorexic illnesses continued throughout the 17th, 18th and 19th centuries.[128]
In the late 19th century anorexia nervosa became widely accepted by the medical profession as a recognized condition. In 1873, Sir William Gull, one of Queen Victoria's personal physicians, published a seminal paper which coined the term anorexia nervosa and provided a number of detailed case descriptions and treatments.[128] In the same year, French physician Ernest-Charles Lasègue similarly published details of a number of cases in a paper entitled De l'Anorexie hystérique.[129]
Awareness of the condition was largely limited to the medical profession until the latter part of the 20th century, when German-American psychoanalyst Hilde Bruch published The Golden Cage: the Enigma of Anorexia Nervosa in 1978. Despite major advances in neuroscience,[130] Bruch's theories tend to dominate popular thinking. A further important event was the death of the popular singer and drummer Karen Carpenter in 1983, which prompted widespread ongoing media coverage of eating disorders.[131]
Etymology
The term is of Greek origin: an- (ἀν-, prefix denoting negation) and orexis (ὄρεξις, "appetite"), translating literally to a nervous loss of appetite.[132]
See also
- List of people with anorexia nervosa
- Eating recovery
- National Association of Anorexia Nervosa and Associated Disorders
- Orthorexia nervosa
- Pro-ana
- Inedia
References
- ↑ Sari Fine Shepphird (2009). 100 Questions & Answers About Anorexia Nervosa. Jones & Bartlett Learning. p. xvi. ISBN 978-1-4496-3079-9.
- 1 2 3 4 5 6 7 8 "What are Eating Disorders?". NIMH. Retrieved 24 May 2015.
- 1 2 3 4 Attia E (2010). "Anorexia Nervosa: Current Status and Future Directions". Annual Review of Medicine. 61 (1): 425–35. doi:10.1146/annurev.med.050208.200745. PMID 19719398.
- 1 2 3 4 5 6 7 8 9 10 Diagnostic and statistical manual of mental disorders : DSM-5 (5 ed.). Washington: American Psychiatric Publishing. 2013. pp. 338–345. ISBN 978-0-89042-555-8.
- ↑ Arcelus, J; Witcomb, GL; Mitchell, A (March 2014). "Prevalence of eating disorders amongst dancers: a systemic review and meta-analysis.". European eating disorders review : the journal of the Eating Disorders Association. 22 (2): 92–101. doi:10.1002/erv.2271. PMID 24277724.
- ↑ Hay, P (July 2013). "A systematic review of evidence for psychological treatments in eating disorders: 2005–2012.". The International Journal of Eating Disorders. 46 (5): 462–9. doi:10.1002/eat.22103. PMID 23658093.
- 1 2 3 4 5 "Feeding and eating disorders" (PDF). American Psychiatric Publishing. 2013. Retrieved 9 April 2015.
- 1 2 British Psychological Society (2004). "Eating Disorders: Core Interventions in the Treatment and Management of Anorexia Nervosa, Bulimia Nervosa and Related Eating Disorders." (PDF): 103. PMID 23346610.
- ↑ Global Burden of Disease Study 2013, Collaborators (5 June 2015). "Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet (London, England). 386 (9995): 743–800. doi:10.1016/S0140-6736(15)60692-4. PMC 4561509
 . PMID 26063472.
. PMID 26063472. - 1 2 3 4 5 Smink, FR; van Hoeken, D; Hoek, HW (August 2012). "Epidemiology of eating disorders: incidence, prevalence and mortality rates.". Current psychiatry reports. 14 (4): 406–14. doi:10.1007/s11920-012-0282-y. PMC 3409365
 . PMID 22644309.
. PMID 22644309. - ↑ GBD 2013 Mortality and Causes of Death Collaborators (17 December 2014). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–171. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604
 . PMID 25530442.
. PMID 25530442. - 1 2 3 4 5 6 Espie J, Eisler I (2015). "Focus on anorexia nervosa: modern psychological treatment and guidelines for the adolescent patient". Adolesc Health Med Ther. 6: 9–16. doi:10.2147/AHMT.S70300. PMC 4316908
 . PMID 25678834.
. PMID 25678834. - ↑ Gull, WW (September 1997). "Anorexia nervosa (apepsia hysterica, anorexia hysterica). 1868.". Obesity Research. 5 (5): 498–502. doi:10.1002/j.1550-8528.1997.tb00677.x. PMID 9385628.
- 1 2 Surgenor LJ, Maguire S (2013). "Assessment of anorexia nervosa: an overview of universal issues and contextual challenges". J Eat Disord. 1 (1): 29. doi:10.1186/2050-2974-1-29. PMC 4081667
 . PMID 24999408.
. PMID 24999408. - 1 2 3 4 Strumia R (2009). "Skin signs in anorexia nervosa". Dermatoendocrinol. 1 (5): 268–70. doi:10.4161/derm.1.5.10193. PMC 2836432
 . PMID 20808514.
. PMID 20808514. - 1 2 3 Miller KK (2013). "Endocrine effects of anorexia nervosa". Endocrinol. Metab. Clin. North Am. 42 (3): 515–28. doi:10.1016/j.ecl.2013.05.007. PMC 3769686
 . PMID 24011884.
. PMID 24011884. - 1 2 Walsh JM, Wheat ME, Freund K (2000). "Detection, evaluation, and treatment of eating disorders the role of the primary care physician". J Gen Intern Med. 15 (8): 577–90. doi:10.1046/j.1525-1497.2000.02439.x. PMC 1495575
 . PMID 10940151.
. PMID 10940151. - ↑ Stargrove MB, Treasure J, McKee DL (2008). Herb, Nutrient, and Drug Interactions: Clinical Implications and Therapeutic Strategies. Elsevier Health Sciences. ISBN 0-323-02964-7. Retrieved 9 April 2015.
- 1 2 3 4 Nolen-Hoeksema S (2013). Abnormal Psychology. New York: McGraw Hill. pp. 339–41. ISBN 978-0-07-803538-8.
- ↑ "Anorexia Nervosa". National Association of Anorexia Nervosa and Associated Disorders. Retrieved 15 April 2014.
- 1 2 Marzola E, Nasser JA, Hashim SA, Shih PA, Kaye WH (2013). "Nutritional rehabilitation in anorexia nervosa: review of the literature and implications for treatment". BMC Psychiatry. 13 (1): 290. doi:10.1186/1471-244X-13-290. PMC 3829207
 . PMID 24200367.
. PMID 24200367. - ↑ Robinson, Paul H. (2006). Community treatment of eating disorders. Chichester: John Wiley & Sons. p. 66. ISBN 978-0-470-01676-3.
- ↑ Haller E (1992). "Eating disorders. A review and update". The Western Journal of Medicine. 157 (6): 658–62. PMC 1022101
 . PMID 1475950.
. PMID 1475950. - ↑ Godier LR, Park RJ (2014). "Compulsivity in anorexia nervosa: a transdiagnostic concept". Front Psychol. 5: 778. doi:10.3389/fpsyg.2014.00778. PMC 4101893
 . PMID 25101036.
. PMID 25101036. - ↑ Crane AM, Roberts ME, Treasure J (2007). "Are Obsessive-Compulsive Personality Traits Associated with a Poor Outcome in Anorexia Nervosa? A Systematic Review of Randomized Controlled Trials and Naturalistic Outcome Studies". International Journal of Eating Disorders. 40 (7): 581–8. doi:10.1002/eat.20419. PMID 17607713.
- ↑ Casper RC (1998). "Depression and eating disorders". Depression and Anxiety. 8 (Suppl 1): 96–104. doi:10.1002/(SICI)1520-6394(1998)8:1+<96::AID-DA15>3.0.CO;2-4. PMID 9809221.
- ↑ Zernig G, Saria A, Kurz M, O'Malley S (24 March 2000). Handbook of Alcoholism. CRC Press. p. 293. ISBN 978-1-4200-3696-1.
- ↑ Sansone RA, Levitt JL (21 August 2013). Personality Disorders and Eating Disorders: Exploring the Frontier. Routledge. p. 28. ISBN 1-135-44280-0.
- ↑ Halmi KA (2013). "Perplexities of treatment resistance in eating disorders". BMC Psychiatry. 13: 292. doi:10.1186/1471-244X-13-292. PMC 3829659
 . PMID 24199597.
. PMID 24199597. - ↑ Swinbourne JM, Touyz SW (2007). "The co-morbidity of eating disorders and anxiety disorders: a review". European Eating Disorders Review : the Journal of the Eating Disorders Association. 15 (4): 253–74. doi:10.1002/erv.784. PMID 17676696.
- ↑ Cortese S, Bernardina BD, Mouren MC (2007). "Attention-deficit/hyperactivity disorder (ADHD) and binge eating". Nutrition Reviews. 65 (9): 404–11. doi:10.1111/j.1753-4887.2007.tb00318.x. PMID 17958207.
- ↑ Wilhelm S, Phillips KA, Steketee G (18 December 2012). Cognitive-Behavioral Therapy for Body Dysmorphic Disorder: A Treatment Manual. Guilford Press. p. 270. ISBN 978-1-4625-0790-0.
- 1 2 Berkman ND, Bulik CM, Brownley KA, Lohr KN, Sedway JA, Rooks A, Gartlehner G (2006). "Management of eating disorders" (PDF). Evid Rep Technol Assess (Full Rep) (135): 1–166. PMC 4780981
 . PMID 17628126.
. PMID 17628126. - ↑ Huke V, Turk J, Saeidi S, Kent A, Morgan JF (2013). "Autism spectrum disorders in eating disorder populations: a systematic review". Eur Eat Disord Rev. 21 (5): 345–51. doi:10.1002/erv.2244. PMID 23900859.
- 1 2 Zucker NL, Losh M, Bulik CM, LaBar KS, Piven J, Pelphrey KA (2007). "Anorexia nervosa and autism spectrum disorders: guided investigation of social cognitive endophenotypes" (PDF). Psychological Bulletin. 133 (6): 976–1006. doi:10.1037/0033-2909.133.6.976. PMID 17967091.
- 1 2 3 4 5 6 7 Rikani AA, Choudhry Z, Choudhry AM, Ikram H, Asghar MW, Kajal D, Waheed A, Mobassarah NJ (2013). "A critique of the literature on etiology of eating disorders". Annals of Neurosciences. 20 (4): 157–161. doi:10.5214/ans.0972.7531.200409. PMC 4117136
 . PMID 25206042.
. PMID 25206042. - ↑ Thornton LM, Mazzeo SE, Bulik CM (2011). "The heritability of eating disorders: methods and current findings". Behavioral Neurobiology of Eating Disorders. Current Topics in Behavioral Neurosciences. 6. pp. 141–56. doi:10.1007/7854_2010_91. ISBN 978-3-642-15130-9. PMC 3599773
 . PMID 21243474.
. PMID 21243474. - ↑ Rask-Andersen M, Olszewski PK, Levine AS, Schiöth HB (2009). "Molecular mechanisms underlying anorexia nervosa: Focus on human gene association studies and systems controlling food intake". Brain Res Rev. 62 (2): 147–64. doi:10.1016/j.brainresrev.2009.10.007. PMID 19931559.
- ↑ Pjetri E, Schmidt U, Kas MJ, Campbell IC (2012). "Epigenetics and eating disorders". Curr Opin Clin Nutr Metab Care. 15 (4): 330–5. doi:10.1097/MCO.0b013e3283546fd3. PMID 22617563.
- ↑ Davis JF, Choi DL, Benoit SC (2011). "24. Orexigenic Hypothalamic Peptides Behavior and Feeding – 24.5 Orexin". In Preedy VR, Watson RR, Martin CR. Handbook of Behavior, Food and Nutrition. Springer. pp. 361–2. ISBN 978-0-387-92271-3.
- ↑ Smitka K, Papezova H, Vondra K, Hill M, Hainer V, Nedvidkova J (2013). "The role of "mixed" orexigenic and anorexigenic signals and autoantibodies reacting with appetite-regulating neuropeptides and peptides of the adipose tissue-gut-brain axis: relevance to food intake and nutritional status in patients with anorexia nervosa and bulimia nervosa". Int J Endocrinol. 2013: 483145. doi:10.1155/2013/483145. PMC 3782835
 . PMID 24106499.
. PMID 24106499. - 1 2 Satherley R, Howard R, Higgs S (Jan 2015). "Disordered eating practices in gastrointestinal disorders". Appetite (Review). 84: 240–50. doi:10.1016/j.appet.2014.10.006. PMID 25312748.
- 1 2 Bern EM, O'Brien RF (Aug 2013). "Is it an eating disorder, gastrointestinal disorder, or both?". Curr Opin Pediatr (Review). 25 (4): 463–70. doi:10.1097/MOP.0b013e328362d1ad. PMID 23838835.
Several case reports brought attention to the association of anorexia nervosa and celiac disease.(...) Some patients present with the eating disorder prior to diagnosis of celiac disease and others developed anorexia nervosa after the diagnosis of celiac disease. Healthcare professionals should screen for celiac disease with eating disorder symptoms especially with gastrointestinal symptoms, weight loss, or growth failure.(...) Celiac disease patients may present with gastrointestinal symptoms such as diarrhea, steatorrhea, weight loss, vomiting, abdominal pain, anorexia, constipation, bloating, and distension due to malabsorption. Extraintestinal presentations include anemia, osteoporosis, dermatitis herpetiformis, short stature, delayed puberty, fatigue, aphthous stomatitis, elevated transaminases, neurologic problems, or dental enamel hypoplasia.(...) it has become clear that symptomatic and diagnosed celiac disease is the tip of the iceberg; the remaining 90% or more of children are asymptomatic and undiagnosed.
- ↑ Quick VM, Byrd-Bredbenner C, Neumark-Sztainer D (1 May 2013). "Chronic illness and disordered eating: a discussion of the literature". Adv Nutr (Review). 4 (3): 277–86. doi:10.3945/an.112.003608. PMC 3650496
 . PMID 23674793.
. PMID 23674793. - ↑ Zandian M, Ioakimidis I, Bergh C, Södersten P (2007). "Cause and treatment of anorexia nervosa". Physiology & Behavior. 92 (1–2): 283–90. doi:10.1016/j.physbeh.2007.05.052. PMID 17585973.
- ↑ Thambirajah MS (2007). Case Studies in Child and Adolescent Mental Health. Radcliffe Publishing. p. 145. ISBN 978-1-85775-698-2. OCLC 84150452.
- ↑ Kaye W (2008). "Neurobiology of Anorexia and Bulimia Nervosa Purdue Ingestive Behavior Research Center Symposium Influences on Eating and Body Weight over the Lifespan: Children and Adolescents". Physiology & Behavior. 94 (1): 121–35. doi:10.1016/j.physbeh.2007.11.037. PMC 2601682
 . PMID 18164737.
. PMID 18164737. - ↑ Lozano GA (2008). "Obesity and sexually selected anorexia nervosa". Medical Hypotheses. 71 (6): 933–940. doi:10.1016/j.mehy.2008.07.013. PMID 18760541.
- 1 2 Herpertz-Dahlmann B, Bühren K, Remschmidt H (2013). "Growing up is hard: Mental disorders in adolescence". Deutsches Arzteblatt international. 110 (25): 432–9; quiz 440. doi:10.3238/arztebl.2013.0432. PMC 3705204
 . PMID 23840288.
. PMID 23840288. - ↑ Wonderlich SA, Brewerton TD, Jocic Z, Dansky BS, Abbott DW (1997). "Relationship of childhood sexual abuse and eating disorders". J Am Acad Child Adolesc Psychiatry. 36 (8): 1107–15. doi:10.1097/00004583-199708000-00018. PMID 9256590.
- ↑ Connors ME, Morse W (1993). "Sexual abuse and eating disorders: A review". The International Journal of Eating Disorders. 13 (1): 1–11. doi:10.1002/1098-108x(199301)13:1<1::aid-eat2260130102>3.0.co;2-p. PMID 8477269.
- ↑ Worthen, Dennis (2001). P & G Pharmacy Handbook. p. 65.
- ↑ Ensminger, Audrey (1983). Foods & nutrition encyclopedia. p. 423.
- ↑ Colman, Andrew (2015). A Dictionary of Psychology. OUP Oxford. p. 851. ISBN 978-0-19-105784-7.
- ↑ Textbook of Clinical Gastroenterology and Hepatology (2 ed.). John Wiley & Sons. 2012. p. 69. ISBN 978-1-118-32142-3.
- 1 2 "Factors That May Contribute to Eating Disorders | National Eating Disorders Association". www.nationaleatingdisorders.org. Retrieved 1 March 2016.
- ↑ Field, Alison E.; Camargo, Carlos A.; Taylor, C. Barr; Berkey, Catherine S.; Roberts, Susan B.; Colditz, Graham A. (1 January 2001). "Peer, Parent, and Media Influences on the Development of Weight Concerns and Frequent Dieting Among Preadolescent and Adolescent Girls and Boys". Pediatrics. 107 (1): 54–60. doi:10.1542/peds.107.1.54. ISSN 0031-4005. PMID 11134434.
- ↑ "Eating disorders and culture". Harvard Mental Health Letter. 20 (9): 7. 1 March 2004. PMID 15044128.
- ↑ Anderson-Fye, Eileen P. and Becker, Anne E. (2004) "Sociocultural Aspects of Eating Disorders" pp. 565-89 in Handbook of Eating Disorders and Obesity, J. Kevin (ed.). Thompson. Hoboken, NJ: John Wiley & Sons.
- ↑ Baum A (2006). "Eating Disorders in the Male Athlete" (PDF). Sports medicine (Auckland, N.Z.). 36 (1): 1–6. doi:10.2165/00007256-200636010-00001. PMID 16445307.
- ↑ "Eating Disorders Anorexia Causes | Eating Disorders". Psychiatric Disorders and Mental Health Issues. Retrieved 1 March 2016.
- ↑ Labre MP (2002). "Adolescent boys and the muscular male body ideal". The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 30 (4): 233–42. PMID 11927235.
- 1 2 Norris ML, Boydell KM, Pinhas L, Katzman DK (2006). "Ana and the Internet: A review of pro-anorexia websites". International Journal of Eating Disorders. 39 (6): 443–7. doi:10.1002/eat.20305. PMID 16721839.
- ↑ Harrison, Kristen (2001). "Ourselves, Our Bodies: Thin-Ideal Media, Self-Discrepancies, and Eating Disorder Symptomatology in Adolescents". Journal of Social and Clinical Psychology. 20 (3): 289. doi:10.1521/jscp.20.3.289.22303.
- 1 2 Kaye WH, Frank GK, Bailer UF, Henry SE, Meltzer CC, Price JC, Mathis CA, Wagner A (2005). "Serotonin alterations in anorexia and bulimia nervosa: new insights from imaging studies". Physiol. Behav. 85 (1): 73–81. doi:10.1016/j.physbeh.2005.04.013. PMID 15869768.
- 1 2 Bergh C, Södersten P (1996). "Anorexia nervosa, self–starvation and the reward of stress". Nature Medicine. 2 (1): 21–22. doi:10.1038/nm0196-21. PMID 8564826.
- ↑ Keating C (2011). "Sex differences precipitating anorexia nervosa in females: the estrogen paradox and a novel framework for targeting sex-specific neurocircuits and behavior". Biological Basis of Sex Differences in Psychopharmacology. Current Topics in Behavioral Neurosciences. 8. pp. 189–207. doi:10.1007/7854_2010_99. ISBN 978-3-642-20005-2. PMID 21769727.
- ↑ Gaudio S, Wiemerslage L, Brooks SJ, Schiöth HB (2016). "A systematic review of resting-state functional-MRI studies in anorexia nervosa: Evidence for functional connectivity impairment in cognitive control and visuospatial and body-signal integration". Neurosci Biobehav Rev. 71: 578–589. doi:10.1016/j.neubiorev.2016.09.032. PMID 27725172.
- ↑ Estour B, Galusca B, Germain N (2014). "Constitutional thinness and anorexia nervosa: a possible misdiagnosis?". Front Endocrinol (Lausanne). 5: 175. doi:10.3389/fendo.2014.00175. PMC 4202249
 . PMID 25368605.
. PMID 25368605. - 1 2 Peat C, Mitchell JE, Hoek HW, Wonderlich SA (2009). "Validity and utility of subtyping anorexia nervosa". Int J Eat Disord. 42 (7): 590–4. doi:10.1002/eat.20717. PMC 2844095
 . PMID 19598270.
. PMID 19598270. - ↑ Singleton, Joanne K. (12 November 2014). Primary Care, Second Edition: An Interprofessional Perspective. Springer Publishing Company. ISBN 978-0-8261-7147-4. Retrieved 9 April 2015.
- ↑ "CBC". MedlinePlus : U.S. National Library of Medicine. Retrieved 31 May 2013.
- ↑ Urinalysis at Medline. Nlm.nih.gov (26 January 2012). Retrieved on 2012-02-04.
- ↑ Chem-20 at Medline. Nlm.nih.gov. Retrieved on 4 February 2012.
- ↑ Lee H, Oh JY, Sung YA, Chung H, Cho WY (2009). "The prevalence and risk factors for glucose intolerance in young Korean women with polycystic ovary syndrome". Endocrine. 36 (2): 326–32. doi:10.1007/s12020-009-9226-7. PMID 19688613.
- ↑ Montagnese C, Scalfi L, Signorini A, De Filippo E, Pasanisi F, Contaldo F (2007). "Cholinesterase and other serum liver enzymes in underweight outpatients with eating disorders". The International Journal of Eating Disorders. 40 (8): 746–50. doi:10.1002/eat.20432. PMID 17610252.
- ↑ Narayanan V, Gaudiani JL, Harris RH, Mehler PS (2010). "Liver function test abnormalities in anorexia nervosa—cause or effect". The International Journal of Eating Disorders. 43 (4): 378–81. doi:10.1002/eat.20690. PMID 19424979.
- ↑ Walder A, Baumann P (2008). "Increased creatinine kinase and rhabdomyolysis in anorexia nervosa". The International Journal of Eating Disorders. 41 (8): 766–7. doi:10.1002/eat.20548. PMID 18521917.
- ↑ BUN at Medline. Nlm.nih.gov (26 January 2012). Retrieved on 2012-02-04.
- ↑ Sheridan AM, Bonventre JV (2000). "Cell biology and molecular mechanisms of injury in ischemic acute renal failure". Current Opinion in Nephrology and Hypertension. 9 (4): 427–34. doi:10.1097/00041552-200007000-00015. PMID 10926180.
- ↑ Nelsen DA (2002). "Gluten-sensitive enteropathy (celiac disease): more common than you think". American Family Physician. 66 (12): 2259–66. PMID 12507163.
- ↑ Pepin J, Shields C (Feb 2012). "Advances in diagnosis and management of hypokalemic and hyperkalemic emergencies". Emerg Med Pract. 14 (2): 1–17. PMID 22413702.
- ↑ "Electroencephalogram". Medline Plus. 26 January 2012. Retrieved 4 February 2012.
- ↑ Madhusmita M, Klibanski A (2011). "The neuroendocrine basis of anorexia nervosa and its impact on bone metabolism". Neuroendocrinology. 93 (2): 65–73. doi:10.1159/000323771. ISSN 1423-0194. PMC 3214929
 . PMID 21228564.
. PMID 21228564. - 1 2 3 Nolen-Hoeksema S (2014). "Eating disorders". Abnormal Psychology (Sixth ed.). New York: McGraw-Hill Education. p. 341. ISBN 978-0-07-803538-8.
- 1 2 Lock JD, Fitzpatrick KK (2009). "Anorexia nervosa". BMJ Clin Evid. 2009. PMC 2907776
 . PMID 19445758.
. PMID 19445758. - ↑ National Institute of Mental Health. "Eating disorders". Retrieved 23 March 2015.
- ↑ National Collaborating Centre for Mental Health (2004). Eating Disorders: Core interventions in the treatment and management of anorexia nervosa, bulimia nervosa and related eating disorders. London, The British Psychological Society and The Royal College of Psychiatrists.
- ↑ Gowers S. G.; et al. (2000). "Impact of hospitalisation on the outcome of adolescent anorexia nervosa". Br J Psychiatry. 176 (2): 138–141. doi:10.1192/bjp.176.2.138.
- ↑ Nolen-Hoeksema, S (2014). Abnormal Psychology (Sixth ed.). McGraw-Hill Education. p. 357. ISBN 978-1-259-06072-4.
- ↑ Blessitt, E., et al. (2015). "Family therapy for adolescent anorexia nervosa." Curr Opin Psychiatry 28(6): 455-460.
- ↑ Garner, David M.; Garfinkel, Paul E. (1997-01-01). Handbook of Treatment for Eating Disorders. Guilford Press. ISBN 978-1-57230-186-3.
- ↑ Whitnet E, Rolfes SR (2011). Understanding Nutrition. United States: Wadsworth Cengage Learning. p. 255. ISBN 1-133-58752-6.
- ↑ Russell, Gerald (1987). "An Evaluation of Family Therapy in Anorexia Nervosa and Bulimia Nervosa". Arch Gen Psychiatry. 44 (12): 1047–56. doi:10.1001/archpsyc.1987.01800240021004. PMID 3318754.
- ↑ le Grange D, Eisler I (2009). "Family interventions in adolescent anorexia nervosa". Child and Adolescent Psychiatric Clinics of North America. 18 (1): 159–73. doi:10.1016/j.chc.2008.07.004. PMID 19014864.
- ↑ "Eating Disorders". National Institute of Mental Health (NIMH). 2011. Retrieved 29 September 2013.
- ↑ "Couples Therapy Helps Combat Anorexia Nervosa". Eating Disorders Review. 23 (6). 2012.
- ↑ Whitfield G, Davidson A (2007). Cognitive Behavioural Therapy Explained. Radcliffe Publishing. ISBN 978-1-85775-603-6. Retrieved 9 April 2015.
- ↑ Keltner NL, Steele D (6 August 2014). Psychiatric Nursing. Elsevier Health Sciences. ISBN 978-0-323-29352-5. Retrieved 9 April 2015.
- ↑ Tchanturia K, Lounes N, Holttum S (2014). "Cognitive remediation in anorexia nervosa and related conditions: a systematic review". Eur Eat Disord Rev. 22 (6): 454–62. doi:10.1002/erv.2326. PMID 25277720.
- 1 2 Pinna F, Sanna L, Carpiniello B (2015). "Alexithymia in eating disorders: therapeutic implications". Psychol Res Behav Manag. 8: 1–15. doi:10.2147/PRBM.S52656. PMC 4278740
 . PMID 25565909.
. PMID 25565909. - ↑ Arcelus J.; et al. (2011). "Mortality rates in patients with anorexia nervosa and other eating disorders. A meta-analysis of 36 studies". Arch Gen Psychiatry. 68 (7): 724–731. doi:10.1001/archgenpsychiatry.2011.74.
- ↑ Robinson P (2012) Avoiding deaths in hospital from anorexia nervosa: the MARSIPAN project. Psychiatrist, 36: 109–13.]
- ↑ Royal_College_of_Psychiatrists (2014). MARSIPAN: Management of Really Sick Patients with Anorexia Nervosa. Second edition. Page 6
- ↑ O'Connor, G. and D. Nicholls (2013). "Refeeding hypophosphatemia in adolescents with anorexia nervosa: a systematic review." Nutr Clin Pract 28(3): 358-364.
- ↑ http://%5Bhttps://www.nice.org.uk/guidance/cg32/chapter/1-Guidance#what-to-give-in-hospital-and-the-community%20NICE%20guideline%20on%20Nutrition%20support%5D
- ↑ Bouquegneau A, Dubois BE, Krzesinski JM, Delanaye P (2012). "Anorexia nervosa and the kidney". Am. J. Kidney Dis. 60 (2): 299–307. doi:10.1053/j.ajkd.2012.03.019. PMID 22609034.
- ↑ Nolen-Hoeksema S (2014). "Eating Disorders". Abnormal Psychology (Sixth ed.). New York: McGraw Hill Education. p. 342. ISBN 978-0-07-803538-8.
- ↑ "Core interventions in the treatment and management of anorexia nervosa, bulimia nervosa and related eating disorders" (PDF). National Collaborating Centre for Mental Health. 2004.
- ↑ Vyver E, Steinegger C, Katzman DK (2008). "Eating disorders and menstrual dysfunction in adolescents". Ann. N. Y. Acad. Sci. 1135: 253–64. doi:10.1196/annals.1429.013. PMID 18574232.
- ↑ Devlin MJ, Walsh BT, Katz JL, Roose SP, Linkie DM, Wright L, Vande Wiele R, Glassman AH (1989). "Hypothalamic-pituitary-gonadal function in anorexia nervosa and bulimia". Psychiatry Res. 28 (1): 11–24. PMID 2500676.
- 1 2 Støving RK, Chen JW, Glintborg D, Brixen K, Flyvbjerg A, Hørder K, Frystyk J (2007). "Bioactive insulin-like growth factor (IGF) I and IGF-binding protein-1 in anorexia nervosa". J. Clin. Endocrinol. Metab. 92 (6): 2323–9. doi:10.1210/jc.2006-1926. PMID 17389700.
- ↑ Misra, Madhusmita; Klibanski, Anne (1 June 2014). "Anorexia nervosa and bone". Journal of Endocrinology. 221 (3): R163–R176. doi:10.1530/JOE-14-0039. ISSN 0022-0795. PMC 4047520
 . PMID 24898127.
. PMID 24898127. - ↑ Kleinman R (1 April 2008). Walker's Pediatric Gastrointestinal Disease. PMPH-USA. ISBN 978-1-55009-364-3. Retrieved 9 April 2015.
- 1 2 Norris ML, Harrison ME, Isserlin L, Robinson A, Feder S, Sampson M (2016). "Gastrointestinal complications associated with anorexia nervosa: A systematic review". Int J Eat Disord. 49 (3): 216–37. doi:10.1002/eat.22462. PMID 26407541.
- 1 2 3 4 5 6 7 Sachs KV, Harnke B, Mehler PS, Krantz MJ (2016). "Cardiovascular complications of anorexia nervosa: A systematic review". Int J Eat Disord. 49 (3): 238–48. doi:10.1002/eat.22481. PMID 26710932.
- 1 2 Goldberg SJ, Comerci GD, Feldman L (1988). "Cardiac output and regional myocardial contraction in anorexia nervosa". J Adolesc Health Care. 9 (1): 15–21. PMID 3335466.
- ↑ Johnson GL, Humphries LL, Shirley PB, Mazzoleni A, Noonan JA (1986). "Mitral valve prolapse in patients with anorexia nervosa and bulimia". Arch. Intern. Med. 146 (8): 1525–9. PMID 3460535.
- 1 2 Hasan TF, Hasan H (2011). "Anorexia nervosa: a unified neurological perspective". Int J Med Sci. 8 (8): 679–703. doi:10.7150/ijms.8.679. PMC 3204438
 . PMID 22135615.
. PMID 22135615. - ↑ Zanetti T (2013). "Epidemiology of Eating Disorders". Eating Disorders and the Skin. pp. 9–15. doi:10.1007/978-3-642-29136-4_2. ISBN 978-3-642-29135-7.
- ↑ Smink FR, van Hoeken D, Hoek HW (2012). "Epidemiology of Eating Disorders: Incidence, Prevalence and Mortality Rates". Current Psychiatry Reports. 14 (4): 406–414. doi:10.1007/s11920-012-0282-y. PMC 3409365
 . PMID 22644309.
. PMID 22644309. - 1 2 Bonci CM, Bonci LJ, Granger LR, Johnson CL, Malina RM, Milne LW, Ryan RR, Vanderbunt EM (2008). "National athletic trainers' association position statement: Preventing, detecting, and managing disordered eating in athletes". Journal of Athletic Training. 43 (1): 80–108. doi:10.4085/1062-6050-43.1.80. PMC 2231403
 . PMID 18335017.
. PMID 18335017. - ↑ Crilly L (2 April 2012). Hope with Eating Disorders. Hay House, Inc. ISBN 978-1-84850-906-1. Retrieved 9 April 2015.
- ↑ Gull WW (1997). "Anorexia nervosa (apepsia hysterica, anorexia hysterica). 1868". Obesity Research. 5 (5): 498–502. doi:10.1002/j.1550-8528.1997.tb00677.x. PMID 9385628.
- 1 2 Pearce JM (2004). "Richard Morton: Origins of Anorexia nervosa". European Neurology. 52 (4): 191–192. doi:10.1159/000082033. PMID 15539770.
- ↑ Espi Forcen F (2013). "Anorexia mirabilis: the practice of fasting by Saint Catherine of Siena in the late Middle Ages". Am J Psychiatry. 170 (4): 370–1. doi:10.1176/appi.ajp.2012.12111457. PMID 23545792.
- ↑ Harris JC (2014). "Anorexia nervosa and anorexia mirabilis: Miss K. R--and St Catherine Of Siena". JAMA Psychiatry. 71 (11): 1212–3. doi:10.1001/jamapsychiatry.2013.2765. PMID 25372187.
- 1 2 Gull, Sir William Withey (1894). T D Acland, ed. Medical Papers. p. 309.
- ↑ Lasègue E (6 September 1873). "On Hysterical Anorexia". Medical Times and Gazette. See also PMID 9385627
- ↑ Arnold, Carrie (2012) Decoding Anorexia: How Breakthroughs in Science Offer Hope for Eating Disorders, Routledge Press. ISBN 0-415-89867-6
- ↑ Arnold, Carrie (29 March 2016). "Anorexia: you don't just grow out of it". The Guardian. Retrieved 29 March 2016.
- ↑ Klein DA, Walsh BT (2004). "Eating disorders: clinical features and pathophysiology". Physiol. Behav. 81 (2): 359–74. doi:10.1016/j.physbeh.2004.02.009. PMID 15159176.
Further reading
- Bailey AP, Parker AG, Colautti LA, Hart LM, Liu P, Hetrick SE (2014). "Mapping the evidence for the prevention and treatment of eating disorders in young people". J Eat Disord. 2 (1): 5. doi:10.1186/2050-2974-2-5. PMC 4081733
 . PMID 24999427.
. PMID 24999427. - Coelho GM, Gomes AI, Ribeiro BG, Soares Ede A (2014). "Prevention of eating disorders in female athletes". Open Access J Sports Med. 5: 105–13. doi:10.2147/OAJSM.S36528. PMC 4026548
 . PMID 24891817.
. PMID 24891817. - Luca A, Luca M, Calandra C (2015). "Eating Disorders in Late-life". Aging Dis. 6 (1): 48–55. doi:10.14336/AD.2014.0124. PMC 4306473
 . PMID 25657852.
. PMID 25657852.
External links
- National Association of Anorexia Nervosa and Associated Disorders
- International Eating Disorder Referral and Information Center
- Anorexia nervosa
- Society of Clinical Psychology--Anorexia
