AV nodal reentrant tachycardia
| AV nodal reentrant tachycardia | |
|---|---|
|
Uncommon AV nodal reentrant tachycardia. In yellow, is evidenced the P wave that falls after the QRS complex. | |
| Classification and external resources | |
| Specialty | cardiology |
| ICD-10 | I47.1 |
| ICD-9-CM | 427.89 |
| eMedicine | med/2955 ped/2535 |
| MeSH | D013611 |
AV nodal reentrant tachycardia (AVNRT), or atrioventricular nodal reentrant tachycardia, is a type of tachycardia (fast rhythm) of the heart. It is a type of supraventricular tachycardia (SVT), meaning that it originates from a location within the heart above the bundle of His. AV nodal reentrant tachycardia is the most common regular supraventricular tachycardia. It is more common in women than men (approximately 75% of cases occur in females). The main symptom is palpitations. Treatment may be with specific physical maneuvers, medication, or, rarely, synchronized cardioversion. Frequent attacks may require radiofrequency ablation, in which the abnormally conducting tissue in the heart is destroyed.
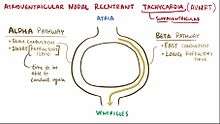
AVNRT occurs when a reentry circuit forms within or just next to the atrioventricular node. The circuit usually involves two anatomical pathways: the fast pathway and the slow pathway, which are both in the right atrium. The slow pathway (which is usually targeted for ablation) is located inferior and slightly posterior to the AV node, often following the anterior margin of the coronary sinus. The fast pathway is usually located just superior and posterior to the AV node. These pathways are formed from tissue that behaves very much like the AV node, and some authors regard them as part of the AV node.
The fast and slow pathways should not be confused with the accessory pathways that give rise to Wolff-Parkinson-White syndrome (WPW syndrome) or atrioventricular reciprocating tachycardia (AVRT). In AVNRT, the fast and slow pathways are located within the right atrium close to or within the AV node and exhibit electrophysiologic properties similar to AV nodal tissue. Accessory pathways that give rise to WPW syndrome and AVRT are located in the atrioventricular valvular rings. They provide a direct connection between the atria and ventricles, and have electrophysiologic properties similar to ventricular myocardium.
Signs and symptoms
The main symptom is the sudden development of rapid regular palpitations. Often, no precipitant is present, although some report development of symptoms in stressful situations, consumption of alcohol or caffeine, or other factors.
In some cases, the onset of the tachycardia is associated with a brief drop in blood pressure. When this happens, the patient may experience dizziness or rarely syncope (fainting). If the heart rate is very fast, and the patient has underlying coronary artery disease (obstruction of the arteries of the heart by atherosclerosis), chest pain similar to angina may be experienced; this pain is band- or pressure-like around the chest and often radiates to the left arm and angle of the left jaw. AVNRT is rarely life-threatening.
Diagnosis
If the symptoms are present while the patient is attending medical care (e.g. emergency department), an electrocardiogram (ECG/EKG) may show typical changes that confirm the diagnosis. If the palpitations are recurrent, a doctor may request a Holter monitor (24-hour or longer portable ECG) recording. Again, this will show the diagnosis if the recorder is attached at the time of the symptoms. Rarely, disabling but infrequent episodes of palpitations may require the insertion of a small microchip-based device (e.g. Reveal Plus) under the skin that continuously record heart activity, and can be read through the skin after an episode. All these ECG-based technologies also enable the distinction between AVNRT and other tachycardias such as atrial fibrillation, atrial flutter, sinus tachycardia, ventricular tachycardia and tachyarrhythmias related to Wolff-Parkinson-White syndrome, all of which may have symptoms that are similar to AVNRT.
Blood tests commonly performed in people with palpitations are:
- thyroid function tests (TFTs) - an overactive thyroid increases the risk of AVNRT
- electrolytes - disturbances in potassium, calcium and magnesium may predispose to AVNRT
- cardiac markers - if there is a concern that myocardial infarction (heart attack) has occurred either as a cause or as a result of the AVNRT; this is usually only the case if the patient has experienced chest pain
Classification
There are several types of AVNRT. The "common form" or "usual" AVNRT utilizes the slow AV nodal pathway as the anterograde limb of the circuit and the fast AV nodal pathway as the retrograde limb. The reentry circuit can be reversed such that the fast AV nodal pathway is the anterograde limb and the slow AV nodal pathway is the retrograde limb. This, not surprisingly, is referred to as the "uncommon form" of AVNRT. However, there is also a third type of AVNRT that utilizes the slow AV nodal pathway as the anterograde limb and left atrial fibers that approach the AV node from the left side of the inter-atrial septum as the retrograde limb. This is known as atypical, or Slow-Slow AVNRT.[1]
Common AVNRT
In common AVNRT, the anterograde conduction is via the slow pathway and the retrograde conduction is via the fast pathway ("slow-fast" AVNRT).
Because the retrograde conduction is via the fast pathway, stimulation of the atria (which produces the inverted P wave) will occur at the same time as stimulation of the ventricles (which causes the QRS complex). As a result, the inverted P waves may not be seen on the surface ECG since they are buried with the QRS complexes. Often the retrograde p-wave is visible, but also in continuity with the QRS complex, appearing as a "pseudo R prime" wave in lead V1 or a "pseudo S" wave in the inferior leads.
Uncommon AVNRT
In uncommon AVNRT, the anterograde conduction is via the fast pathway and the retrograde conduction is via the slow pathway ("fast-slow" AVNRT).
Multiple slow pathways can exist so that both anterograde and retrograde conduction are over slow pathways. ("slow-slow" AVNRT).
Because the retrograde conduction is via the slow pathway, stimulation of the atria will be delayed by the slow conduction tissue and will typically produce an inverted P wave that falls after the QRS complex on the surface ECG.
Treatment
An episode of supraventricular tachycardia (SVT) due to AVNRT can be terminated by any action that transiently blocks the AV node. Various methods are possible.
Vagal maneuvers
Some people with known AVNRT may be able to stop their attack by using various tricks to activate the vagus nerve. This includes carotid sinus massage (pressure on the carotid sinus in the neck) or the Valsalva maneuver (increasing the pressure in the chest by attempting to exhale against a closed airway).
Medication
Medical therapy can be initiated with AV nodal slowing drugs such as adenosine (which is a pharmacologic cardioversion), beta blockers or non-dihydropyridine calcium channel blockers (such as verapamil). Numerous other antiarrhythmic drugs may be effective if the more commonly used medications have not worked; these include flecainide or amiodarone. Both adenosine and beta blockers may cause tightening of the airways, and are therefore used with caution in people who are known to have asthma.
Cardioversion
In very rare instances, cardioversion (the electrical restoration of a normal heart rhythm) is needed in the treatment of AVNRT. This would normally only happen if all other treatments have been ineffective, or if the fast heart rate is poorly tolerated (e.g. the development of heart failure symptoms, low blood pressure or coma).
Electrophysiology
After being diagnosed with AVNRT, patients can also undergo an Electrophysiology (EP) study to confirm the diagnosis. Catheter ablation of the slow pathway, if successfully carried out, can potentially cure the patient of AVNRT.
Pacemaker-mediated tachycardia
A separate form of AV nodal reentrant tachycardia is pacemaker-mediated tachycardia (PMT), a possible complication of dual-chamber artificial pacemakers. In PMT, the artificial pacemaker forms the anterograde (atrium to ventricle) limb of the circuit and the atrioventricular (AV) node forms the retrograde limb (ventricle to atrium) of the circuit.[2] Treatment of PMT typically involves reprogramming the pacemaker.[2]
See also
References
- ↑ http://lifeinthefastlane.com/2009/09/avnrt-ecg/
- 1 2 eMedicine > Pacemaker-Mediated Tachycardia Author: Brian Olshansky, MD. Coauthor(s): Chirag M Sandesara, MD; Noel G Boyle, MB, BCh, MD, PhD. Updated: Jun 17, 2008
External links
- AVNRT Clinical Cases from Life in the Fast Lane Medical Blog
- Supraventricular Tachycardia: Diagnosis and Management from Mayo Clinic Proceedings
